Infart ECGs
Ischemic, injury & necrosis
Phases of Evolution of an acute transmural MI

Phase 1 - importance of rapid intervention
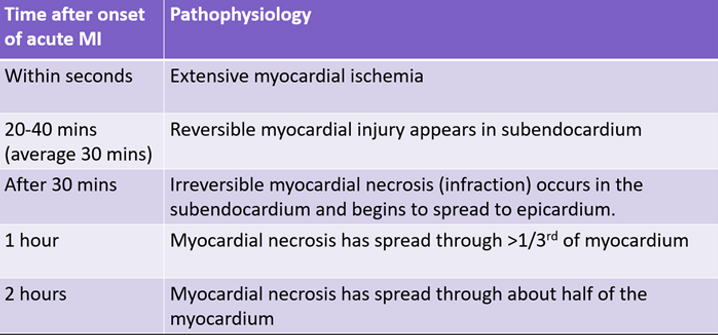

Phase 2 - importance of rapid intervention


Ischemia
ST depression
•Upward sloping = non specific for ischemia
•Downward sloping/horizontal >1mm in 2+ leads
•Widespread ST depression may reflect reciprocal changes

T wave inversion
•1mm deep inversion in 2+ leads which have dominant R waves
•Dynamic: previously not seen on other ECGs
•Caused by delay or change in direction of repolarisation of the myocardium due to hypoxia.
•They may be abnormally tall/peaked or deeply inverted
•QT intervals may also be prolonged

Wellens syndrome
A pattern of inverted or biphasic T waves in V2-V4 highly specific for critical LAD stenosis
-
Type A – biphasic (~25% of cases)
-
Type B (~75% cases)
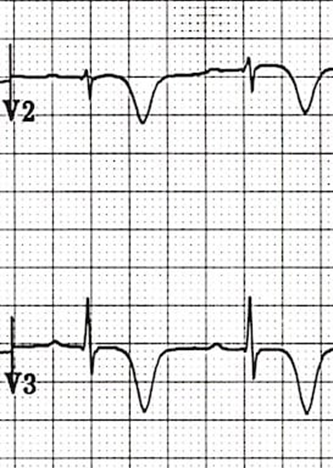
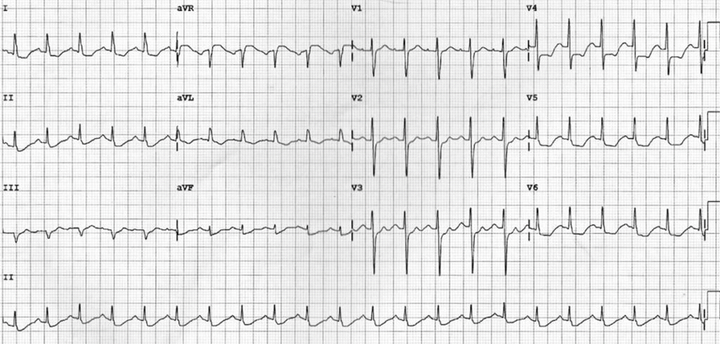
Wellens type A

Wellens type B
De winter T wave
ST depression (can be upsloping, but >1mm)
Peaked T waves in precordial leads
~2% of acute LAD occlusions

Injury
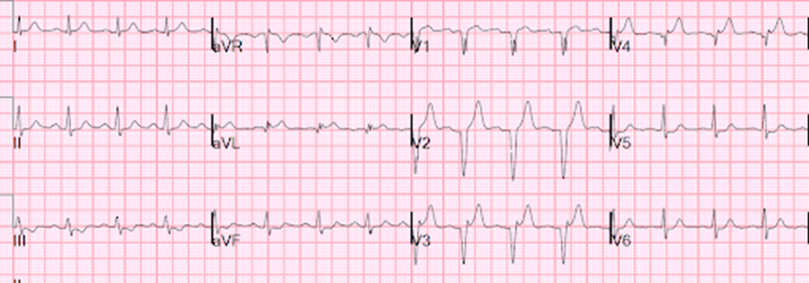
ST elevation and reciprocal depression
•ST elevation is “the current of injury” an electrical manifestation of the inability of cardiac cells “injured” by severe ischemia to maintain a normal resting membrane potential in diastole
•Reciprocal ST depression reflect the myocardium directly opposite the are of ischemia

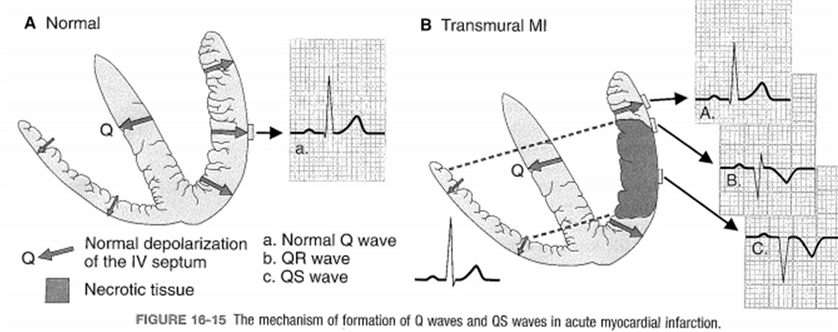
Necrosis
•Q wave development - ~50% of pts
•Usually develop ~8-12hrs after MI onset- max size ~24-48 hrs
•“window” through to opposite non infarcted wall (electrically inert)
Regional pattern changes on ECG


Anterior infarct


Acute anterior infarct

Old anterior infarct
Extensive anterior infarct


Old extensive anterior infarct

Antero-septal


Septal


Lateral


high lateral

Antero-lateral


LMCA

Inferior

Acute inferior infarct

Old inferior infarct

Posterior


RV


Arrhythmias in infarcts
Bradyarrhythmias
Sinus node dysfunction
•Atrial branch of RCA (~55% of pts)
•Proximal branch of LCx (~45% of pts)
AV blocks
•RCA (AVN and proximal HIS)
•LAD (distal HIS)
Bundle branch blocks
•LAD (LPF, LAF, RBB)
•RCA (LPF)
Occurs in ~0.3% - 18% of AMI pts
May also be vagally mediated
May require temporary pacing
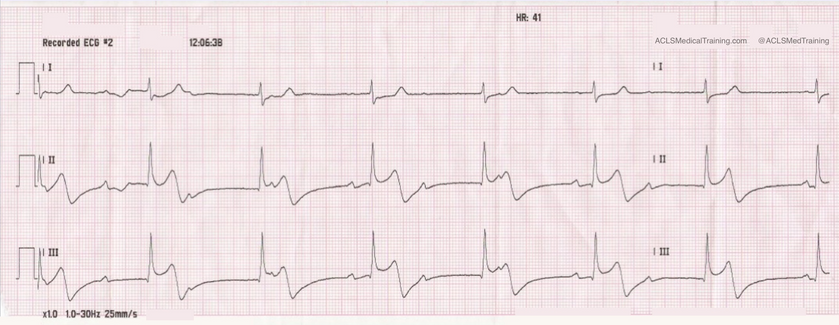
Sinus bradycardia

Wenckebach

2nd degree AV block (2:1 pattern)

sinus with CHB - junctional escape
Sinus with CHB - ventricular escape

High grade AV block - ventricular escape

AF with CHB

Tachyarrhythmias
Sinus tachycardia
•May be due to elevated sympathetic nervous activation
•May be a result of cardiogenic shock (overcompensating hypotension)
•Response to administered medications (adrenaline/atropine)
Ventricular arrhythmias
•May require defibrillation or Amiodarone infusion
Atrial fibrillation
•Between 6-20% of AMI
Reperfusion Arrhythmia –accelerated idioventricular/VPBs
•Consequence of cellular humoral reactions resulting from opening of coronary artery
Sinus tachycardia

Ventricular tachycardia

Torsades / Polymorphic VT

Ventricular fibrillation

Reperfusion arrhythmia

Reperfusion arrhythmia





