VT/VPB ablation

VT/VPB basics
Cause
-
VT/VPB are generally categorised into being idiopathic or scar related.
-
Idiopathic VTs generally occur in structurally normal hearts and are often automatic or triggerred.
-
Scar related VTs are re-entry in nature and are usually assoctaed with abnormal hearts (these patients usually have ICDs implanted).
Indication for ablation
idiopathic VTs,
a patient either must have symptomatic frequent VPBs, or frequent VPBs resulting in LV dysfunction.
Scar-related VTs
VT ablation is considered much more high risk and is often only done as a last resort.
Ideally the patient is treated with medical therapy.
If medical therapy is unsuccessful and patient is still experiencing recurrent VT, ablation can be considered.
VT/VPB ablation
Ablation
Success rates
>90% for idioventricular VT/VPBS (structurally normal heart)
~ Significantly lower (~50-70%) for structurally pts with structurally abnormal hearts - scar related VTs.
Complications
Complications depend on location and type (idiopathic/scar related) of the arrhythmia.
Equipment
-
Depending on location may be venous only (RV) or both venous and arterial (LV)
-
Often involves a coronary sinus decapolar catheter
-
May involve a JSN for RV pacing
-
If ablation is to be performed RF ablation irrigation is often chosen (deeper lesions).
-
3D mapping can be utilised if desired with HD mapping catheter
Mapping the origin
Depending on the type of VT/VPB, there are several ways to map.
Activation timing:
mapping the earliest ventricular signal to the onset of the QRS (in tachy/during the VPB). This is ideally >30ms early to ECG. Bracketing the earliest activation is important to ensure the absolute earliest signal is found.
Late activation signals (late diastolic potentials) during VT can also be targeted during VT (useful for reentry VTs).

RVOT activation map (Left: LAO; Right; left lateral)
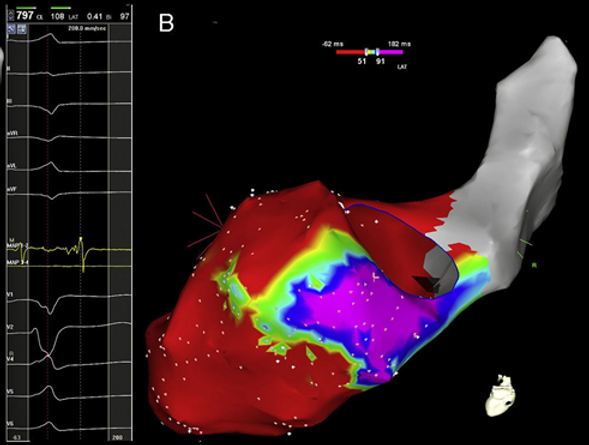
Late potentials during VT - mid/basal inferior LV
Pace mapping:
pacing from the catheter tip to see if the evoked response in 100% identical to the intrinsic VPB/VT. There is issues with this technique, as it is dependent on how much of the myocardium is captured.

3 sites looking at pace mapping
Entrainment mapping:
Entrainment mapping is the gold standard to be used during a re-entry VT. This must be done during tachycardia (and therefore the patient should be stable during the arrhythmia- this can be difficult). Ventricular entrainment is performed ~20-30ms faster than the VT CL. Tachycardia should continue post entrainment is ceased.
PPI-TCL
should be <30ms to be in the circuit. However, being in the citcuit (short PPI-TCL) does not indicte whether you are in the inner loop (where to ablate), the outer loop, or in a bsytander part of the circuit.
100% match score
should occur (concealed entrainment) when pacing is in the inner loop tachycardia circuit.
If there is 100% match score but PPI-TCL is >30ms, this is an adjacent bystander.
If there is cocealed fusion and PPI-TCL <30ms, the stim-QRS is then evaluated. Specifically, the
(S-QRS/VT CL) x 100 is calculated
-If the (S-QRS/VT CL) x 100 is long (>70%), this will be the inner loop.
-If the (S-QRS/VT CL) x 100 is short(<30%), this will be the exit site
-If the (S-QRS/VT CL) x 100 is somewhere in the middle (30-70%), this will be along the central isthmus. This is the desired location to ablate
SEE IMAGE BELOW

3 sites looking at pace mapping
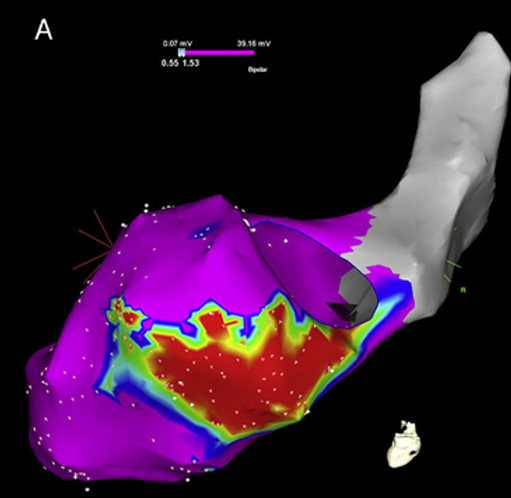
Scar/voltage mapping:
this can be useful for patients with re-entry/scar related VT where the patient is too unstable to map during VT, or VT is uniducible on the day. Areas of low voltage (scar) may be shown to be in patches of area, which can set up for arrhythmias. Scar homogenisation can be performed to elimiate the isthmus responsible for the VT.