Atrial flutter (AFl)

AFl basics
Typical AFl
-
When talking about typical atrial flutters, this referes to flutters which utilise the cavo tricuspid isthmus (CTI), also known as CTI dependent flutters.
-
CTI flutter presentations account for >90% of all atrial flutters
-
A CTI flutter ablation is typically a straight forward procedure with high success rate >90%, and low complication risk <1%


Typical AFl with saw tooth appearance on ECG

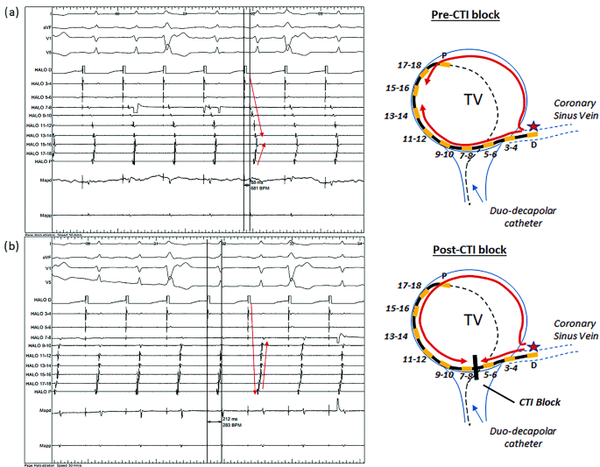
Typical CTI AFl and post ablation block

Atypical AFl
-
Atypical atrial flutters are any flutters outside the CTI.
-
These flutters are often associated with scar (often post surgical (e.g., cardiac surgery, post PVI ablation, etc) or scar developed by certain conditions (e.g., sarcoid))
-
Can be difficult to map and ablate
-
Often are left sided
-
Multiple atrial circuits may be involved

Examples of atypical atrial flutter circuits

Atypical AFl with isoelectric segments on ECG
Mitral annular AFl
Atrial entrainment in atrial flutter
-
Atrial entrainment is a manouvre utilised during atrial flutter to determine if the pacing site is part of the atrial flutter circuit.
-
This is done by pacing at any point in the atrium 20-30ms faster that the TCL. The tachycardia must continue after (exact same rhythm- same activation- same rate).
-
The PPI-TCL can then be evaluated.
-
If PPI-TCl is <30ms this indicates that the pacing location is in the circuit.
-
The greater the PPI-TCL, the further away from the circuit the catheter is.
-
Other activation patterns can be viewed in terms of conceled or manifest patterns to determine if the pacing site is similar/different location to the atrial flutter.
for example: a typical atrial flutter will have concentric atrial activation across the CS (CSp to CSd). Pacing from the CTI region will show the same activation pattern in the CS (concealed fusion). However pacing from the lateral LA will result in eccentric CS activation (CSd to CSp) and will demonstrate manifest activation.

AFl ablation
Equipment
-
Venous access multiple sites
-
Often a decapolar coronary sinus catheter is used
-
A second decapolar or duodecapolar catheter may be utilised to sit along the lateral RA for typical CTI flutters
-
May need transeptal equipment if left sided (sheath and needle - multiple (2) punctures may be performed - Dr dependent)
-
Ablation catheter
-
+ / - 3D mapping catheter (almost always used for atypical AFl)
Procedure - CTI ablation
-
Patient does not need to be in in atrial flutter for ablation to be performed.
-
Venous access obtained
-
Coronary sinus catheter +- other diagnostic catheters positioned
-
3D mapping may be used, and 3D geometry of the right atrium can be collected
-
If in atrial flutter, a reentrant/activation may can be collected with 3D mapping.
-
Tachycardia termination during ablation is a good sign if there is A-A cycle length increase seen prior to termination (not terminated by atrial ectopy at a faster rate)
-
Gaps in the line can be found if there are tight doubles on the ablation EGM (see picture below)

TICT
- Entrance and exit block is confirmed by pacing from either side of the CTI and measuring the time and activation pattern that is used to conduct across this area. This is known as the trans isthmus conduction time (TICT) and it can be measured pre, during and post ablation when the patient is in sinus rhythm.
- TICt is measured by pacing from proximal CS to low lateral RA and in the reverse. Prior to ablation this should be relatively slick (~60 ms).
- The TICT should increase as the ablation line is performed (usually to > double the baseline TICT).
- To prove bidirectional block, the TICT should be shorter from higher up the lateral RA compared to the lower lateral RA to the proximal CS and vice versa.
- This demonstrates that although low lateral RA is physically closer to the CSp, activation is blocked through the CTI and therefore has to go the opposite direction up the septum across the superior RA to the lateral RA, and therefore high lateral RA will be earlier than low lateral RA (and same when pacing in reverse).
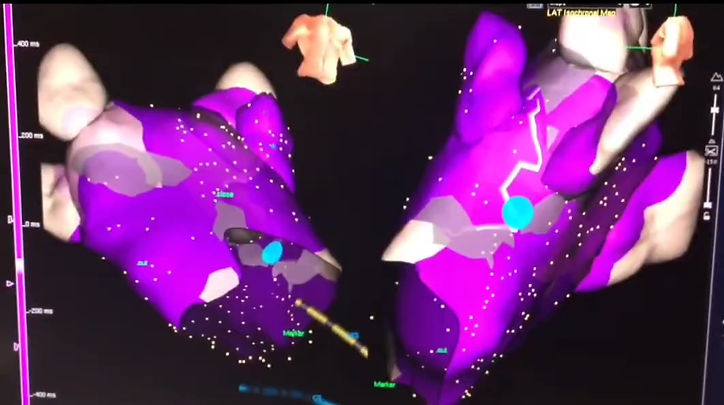
Procedure - atypical atrial flutter ablation
-
Patient must be in the atrial flutter to determine the location of the circuit.
-
Venous access obtained
-
Coronary sinus catheter +- other diagnostic catheters positioned
-
3D geometry & reentry map of the right atrium can be collected and atrial entrainment may be utilised to prove/disprove RA involvement in flutter or confirm location.
-
If thought to be left sided, transeptal puncture performed
-
3D geometry and reentry map of the left atrium can be collected and atrial entrainment may be utilised to confirm circuit.
-
Shortest ablation line is chosen.
-
Tachycardia termination during ablation is a good sign if there is A-A cycle length increase seen prior to termination (not terminated by atrial ectopy at a faster rate)
-
Entrance and exit block is confirmed across the line (similar principle to TICT as discussed above from either side of the line, in both directions.




