AVNRT

AV node basics
AV node physiology
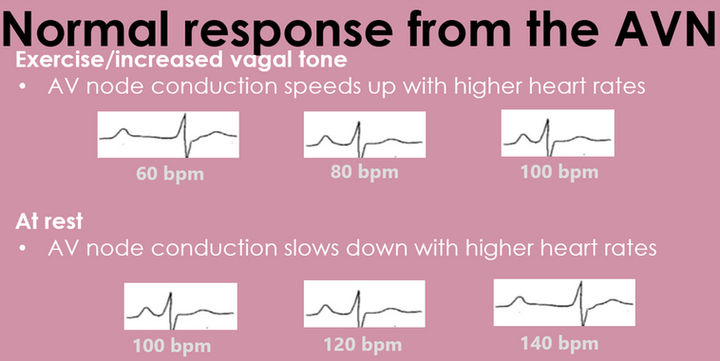
With exercise, AV nodal conduction speeds up (shortens in ms)
However, when at rest, AV nodal conduction slows down (lengthens in ms) when pacing at higher rates.
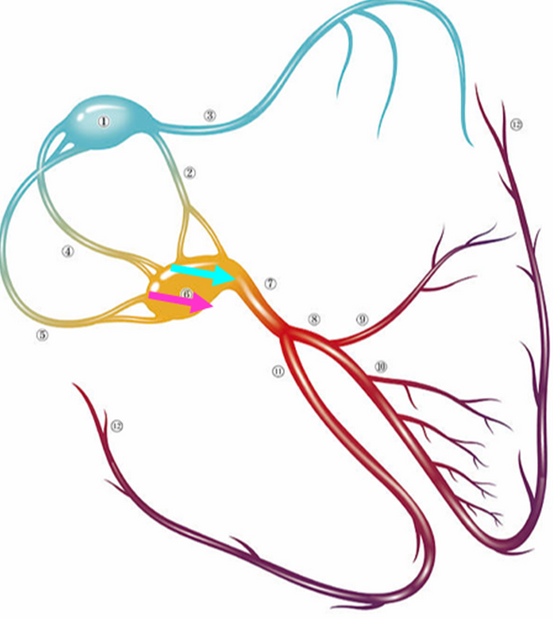
Majority of the population have single AV node physiology. This means that there is one channel from atrial conduction to travel to the ventricle through the AV node.
In ~20-25% of the population, dual AV node physiology exists. This is when there are 2+ channels around the AV node that allow conduction from the atrium to the ventricle.
In dual AV node physiology, there are differences in conduction speeds (often termed fast and slow) and there can be differences in effective refractory periods.
Preferential conduction from the atrium to the ventricle will occur via the faster conduction pathway.
Single AV node physiology

Dual AV node physiology
Dual AV node physiology and AVNRT
Although 25% of the population has dual AVN physiology, only 0.1% of the population present with AVNRT.
For AVNRT to occur, the patient must have retrograde AVN conduction, a difference in the ERPs of the different pathways and needs a trigger.
An atrial premature beat is often a trigger for typical AVNRT (ventricular ectopics may trigger too and are can be more effective in induction of atypical AVNRT compared to atrial premature beats).
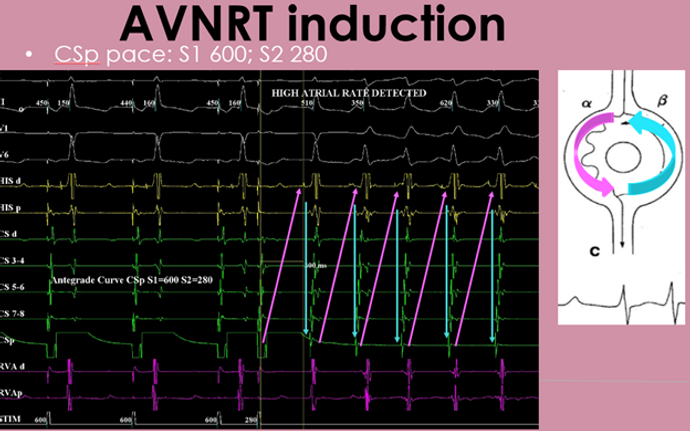
The below diagram shows a very simplified image of dual AV node physiology and AVNRT induction.
Figure A demonstrates an atrial impulse travelling down both fast (blue) and slow (pink) pathways simultaneously. Only the fast pathway causes a ventricular response, as by the time the slow pathway reaches the distal point of the node, the ventricle is refractory.
Figure B: demonstrates an atrial ectopic beat travelling down the slow pathway causing a ventricular response and a prolonged AV interval. The fast pathway was refractory to the atrial ectopic at that specific rate (difference in pathway ERPs) and therefore did not have any effect on the ventricle.
Figure C: the 1st beat of the tachycardia occurs like Figure B described above. This time however, when the slow pathway reaches the distal part of the node, the fast pathway is no longer refractory and can except a retrograde impulse back to the atrium. This cycle continues resulting in sustained AVNRT.or

click below for video

click below for video

AVNRT Ablation
Equipment
-
Often venous access only
-
Often involves a coronary sinus decapolar catheter
-
1-3 other quadripolar JSN catheters may be used depending on Dr preference. This traditionally are placed into the high right atrium, HIS and RV apex. If only 1 JSN is used it can be moved around to several positions to perform testing and analyse results.
-
If ablation is to be performed RF ablation (either non irrigated or irrigated) can be used. Focal cryothermy ablation may be considered if there is higher risk of AV block (damage to fast pathway) and is often used in paediatric patients.
-
3D mapping can be utilised if desired
Basic EP study procedure
-
In order for AVNRT to occur, retrograde conduciton must exist. If there is VA dissociation at rest, Isuprel is usually administered.
-
Retrograde/ventricular pacing protocols are performed to determine
-if there is retrograde conduction
-is the atrial activation pattern consistent with nodal conduction (usually midline - termed concentric), or via an accessory pathway (eccentric)
-is the VA conduction decremental (consistent with AP or has not reached relative refractory period (excessive sympathetic tone/slick AV/VA)) or non decremental (consistent with AV node - rare APs)?
-If it is unclear whether retrograde conduction is via AV node or septal pathway there are tachniques to help determine this.
Click here for more info on determining retrograde conduction
-
Antegrade/atrial pacing protocols are performed to determine
-if there is single or dual AV node physiology
-is there any increase in pre-excitation (AP)
-
Tachycardia induction is desired to diagnose the mechanism of the arrhythmia.
Testing for duality
-
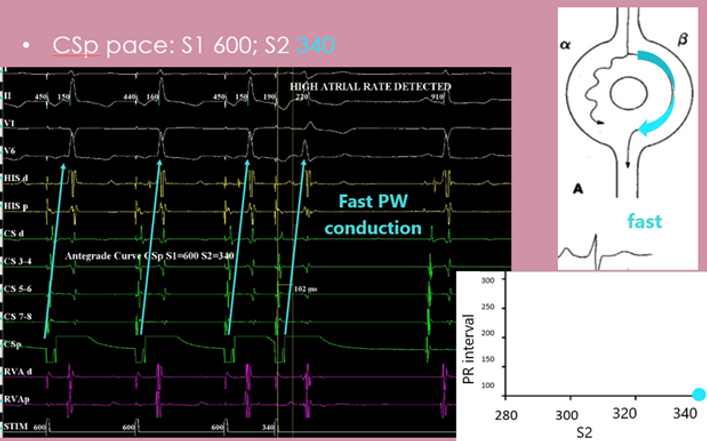
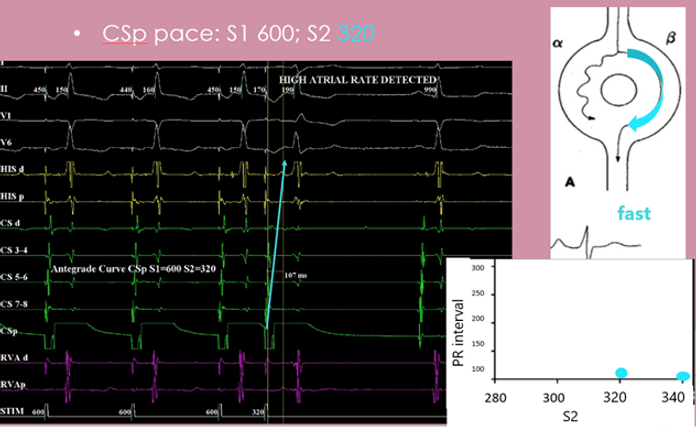
Performing a series of atrial paced extras is a great way to assess if dual AV node physiology exists.
-
The S2 will be decremented until one of the following things occurs
-there is no atrial conduction (AERP
-there is no AVN conduction (AVN ERP) or
-tachycardia is induced
-
If there is single AV node physiology, there will be gradual increase in the AH interval until ERP is reached (picture below)
-
If there is dual AV node physiology, there will be a jump in AH interval (defined as >50ms) when the fast pathway hits refractory and conduction is occurring via the slow pathway (picture below).
Single AV node physiology

Dual AV node physiology

Example of antegrade curve with dual AV node physiology
Example of antegrade curve with dual AV node physiology


Ablation
Success rates
95-98%
Complication
Low <1%
Risk of damage to AV node (may require PPM implant)
Slow pathway locations
-
Majority (>94%) of slow pathways involve a right inferior extension (RIE)
-
Less commonly (<5%) there may be a left inferior extension (LIE) which is located more left sided close to the septum (may have eccentric VA conduction depending on CS catheter position)
-
There is an even rarer occurrence (<1%) of an infero-lateral LA extension (IL-LA) (will have eccentric VA conduction on CS catheter)

Targeting the RIE slow pathway location
-
The triangle of Koch is used to locate the slow pathway.
-
The triangle of koch includes
-Coronary sinus ostium (posterior)
-Septal leaflet of tricuspid valve (anterior/inferior)
-Tendon of Todaro (superior)
-
The AV node is positioned superiorly and anteriorly at the apex of the triangle.
-
The fast pathway is located closer to this region and is generally more superior
-
The slow pathway is located closer to the CS OS and is more inferior.

Ablating the slow pathway
-
X-ray alone with EGMs can be used to ablate the slow pathway region.
-
If 3D mapping is used the slow pathway region may be located by
-Anatomical location
-Voltage mapping during sinus rhythm (low voltage bridge)
-Activation mapping during sinus rhythm ( Slow pathway Late Activation Mapping - SLAM)

Slow pathway EGM appearance
-ensure there is no HIS signal on the ablation catheter
-the ratio A to V is often 1:5 - 1:3
-the lower the ratio (e.g., 1:3) the closer to the fast conduction
-the atrial component will be low amplitude and fractionated /multicomponent (bump and a spike)

correlating fast and slow pathway areas on a low voltage bridge map (left) and SLAM (right)
-superior line = fast - mid/inferior line = slow
Ablation responses
During ablation a good response to damaging the slow pathway is to see slow consistent junctional rhythm that speeds and slows.
Immediately come off ablation if there is fast junctional acceleration or any prolongation in the PR interval (this is consistent with damage to the fast inputs)




