Accessory pathways (AP)
Accessory pathway (AP) basics
AP physiology
APs are an extra band across the AV sulcus allowing for extra nodal conduction.
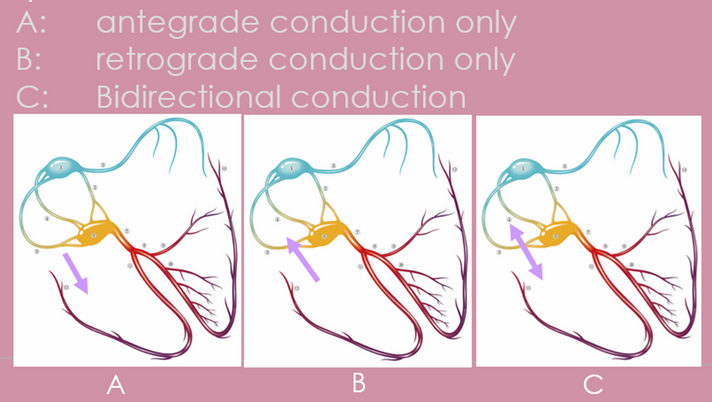
Pathways may conduct either
-
Antegrade only
-
Retrograde only
-
Bidirectional (most common)
AVRT can be antidromic or orthodromic
-
Antidromic AVRT is when atrial activation travels to the ventricle via the AP and back to the atria via the AV node (VA conduction). WIll have a broad complex
-
Orthodromic AVRT is when atrial actuvation travels to the ventricle via the AV node and back to the atria via the AP. Will be narrow complex unless aberrancy is present.
All pathways can be involved in AVRT
-
Antegrade only: antidromic AVRT only
-
Retrograde only: orthodromic AVRT only
-
BIdirectional: either antidromic or orthodromic AVRT (but majority are orthodromic)
Antegrade conducting pathways can show pre-excitation on ECG (manifest) (0.1-0.4% incidence)
WPW involves pre-excitation on ECG with reported palpitations.
~30% of pathways are concealed (no evidence of pre-excitation on ECG)
Degree of pre-excitation depends on speed of AV node conduction and location of accessory pathway (proximity to AV node)
5-10% of patients have multiple pathways (sometimes associated with Ebstein anomaly)
~7% of patients have decremental pathways.
Atrial fibrillation is reported to occur in 15% of patients with WPW.
Unlike the AV node which only allows certain rates to conduct from the atria to the ventricle, some accessory pathways can have very rapid conduction. When a patient with a rapidly conducting AP goes into AF, there rates are so fast that there is potential for syncope and degeneration into VF and sudden cardiac death.
If pre-excitation is seen on ECG, even if the patient is asymtomatic, the patient can still undergo EP study to assess the speed of the pathway. Even though the pathway may not be responsible in a tachycardia circuit (AVRT), it may still need to be ablated to help minimse the risk of sudden cardiac death due to rapid conduction in AF.
There are several types of AP
-majority are atrioventricular (.1-3% of the population)
Other rare types include
-Atriofasicular
-Nodoventricular/nodofasicular (Mahaim fibers)
-Fasciculoventricular (HIS to myocardium). Will have intermittent pre-excitation but are mot dangerous (risk of SCD) because they are below the AV node.
-Atrionodal (RA to node)
Some pathways may be slow conducting (long local VA conduction; like PJRT)
Some pathways may be oblique, and therefore their atrial and ventricular insertion sites may be relatively separate along the annulus.

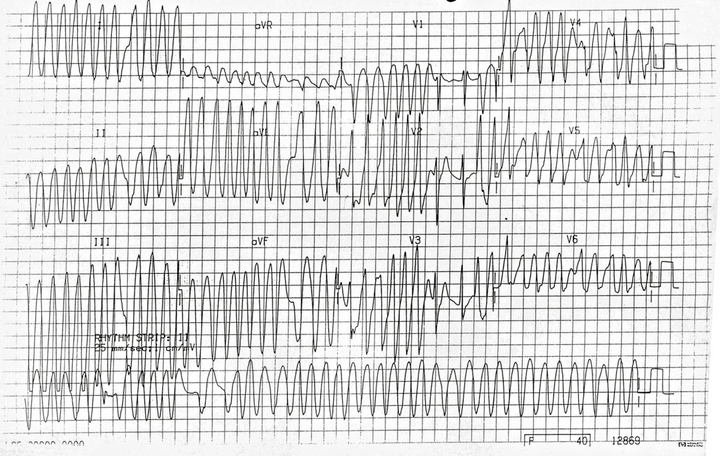
Rapid pathway conduction in AF
AP ablation
Equipment
-
Often venous access only - unless a retrograde aproach is used to ablate a left sided pathway
-
Often involves a coronary sinus decapolar catheter
-
1-3 other quadripolar JSN catheters may be used depending on Dr preference. This traditionally are placed into the high right atrium, HIS and RV apex. If only 1 JSN is used it can be moved around to several positions to perform testing and analyse results.
-
If ablation is to be performed RF ablation (either non irrigated or irrigated) can be used. Focal cryothermy ablation may be considered if there is higher risk of AV block (AP close to AV node)
-
3D mapping can be utilised if desired
Basic EP study procedure
-
Retrograde/ventricular pacing protocols are performed to determine
-if there is retrograde conduction
-is the atrial activation pattern consistent with nodal conduction (usually midline - termed concentric), or via an accessory pathway (eccentric)
-is the VA conduction decremental (consistent with AP or has not reached relative refractory period (excessive sympathetic tone/slick AV/VA)) or non decremental (consistent with AV node - rare APs)?
-If it is unclear whether retrograde conduction is via AV node or septal pathway there are tachniques to help determine this.
Click here for more info on determining retrograde conduction
-
Antegrade/atrial pacing protocols are performed to determine how rapidly conducting the AP is
-
Some guidelines suggest ablating the AP if it can conduct <250ms
-
If there is documented tachycardia. induction is desired to diagnose the mechanism of the arrhythmia.
Ablation
Success rates
90-95%
Complications
Complications depend on location of the pathway
(e.g., left sided AP may result in transeptal puncture (risks associated); AP may be close to AV node)
Mapping the pathway
Depending on the pathway properties, there are 3 different ways to map an AP
-
Earliest V signal to the onset of the delta wave (at max pre-excitation)
-
Earliest A signal during orhtodromic AVRT (pure AP conduction)
-
Earliest A during ventricular pacing (may have some degree of fusion up the AV node depending on the proximity)
Mapping can be performed at either the ventricular insertion point or the atrial insertion point (or both)
Bracketing the pathway is important to ensure the absolute earliest signal is found.





