Atrial arrhythmias
Premature atrial complexes / atrial ectopy
-
When an early atrial beat (outside the sinus node) occurs prior to the next expected sinus beat.
-
Either enhances automaticity or reentry
-
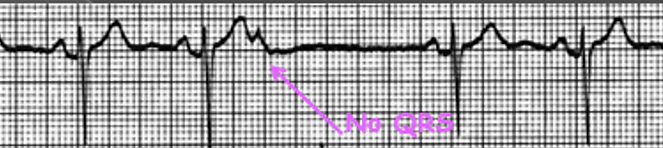
The ectopic may result in a following QRS or may be non conducted through the AV node.
-
Aberrant conduction may occur if the bundle branches are not fully recovered from the previous beat.
-
These beats may occur in pairs (couplets), in threes (triplets) or in brief runs (salvos)
Causes
-
increase in sympathetic tone
-
infections
-
stimulants (caffeine, tabacco, alcohol)
-
hypoxia
-
Medication related (Digitalis, epinephrine, etc)
-
Atrial disease/defect (septal defect, dilated atria, etc)
-
cardiovascular disease
Single atrial ectopic

Non conducted atrial ectopic
Atrial ectopic with aberrant conduction

Atrial couplet

Atrial triplet

Atrial run/salvo

Atrial flutter
Macro reentry circuit in the atrium.
Often associated in patients with
-
cardiomyopathy
-
rheumatic heart disease
-
coronary/hypertensive heart disease
-
hypoxia
-
heart failure
-
alcoholism
-
thyrotoxicosis
-
atrial dilatation
-
previous cardiac surgery/ablation
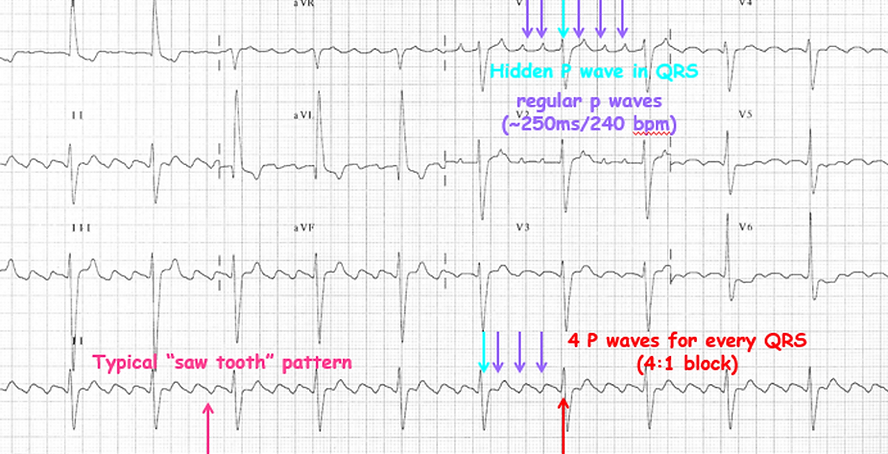

2:1 AFl

AFl with variable block

AFl with high grade block

Atrial fibrillation
Characterised by fast, irregular and chaotic atrial signals firing/fibrillating.
Often results in an irregular ventricular rhythm due to the variability of the atrial signals bombarding the AV node.
Commonly asociated with patients with
-
rheumatic heart disease
-
obesity
-
hypertensive/coronary artery disease
-
thyrotoxicosis
-
heart failure
-
cardiomyopathy
-
dilated atria
-
pulmonary disease


AF with rapid conduction

AF with slow conduction

Pre-excited AF

Atrial tachycardia
A focal or reentry arrhythmia originating from a specific part of the atrium.
Often associated in patients with
-
coronary artery disease
-
hypoxia
-
rheumatic heart disease
-
chronic lung disease
-
metablic abnormalities


Supraventricular tachycardia - SVT
A reentry arrhythmia involving 2+ pathways across the AV groove.
Usually begins with an ectopic (can be atrial or ventricular).
Can be terminated with vagal maneouvres or administration of Adenosine (AV nodal blocking agent).
May require ablation.
AVNRT (AV nodal reentry tachycardia)
-
Reentry circuit around the AV node
-
Patient requires dual AV node physiology for the arrhythmia to occur
-
Tachycardia may have intermittent lower common blcok where there are 2 atrial events for every 1 ventricular event, or upper common block (very rare) where there are 2 ventricular events for every 1 atrial event,
There are 3 types of AVNRT
-
slow-fast: most common which involves antegrade conduction down the slow pathway and retrograde conduction up the fast pathway.
-
fast-slow: involves antegrade conduction down the fast pathway and retrograde conduction up the slow pathway.
-
Slow-slow: involves antegrade and retrograde conduction up/down 2 slow pathways.
AVRT (Atrioventricular reentry tachycardia)
-
Reentry circuit which utilises an accessory pathway
-
May utilise 2 accessory pathways or 1 accessory pathway with the AV node as the 2nd limb.
There are 2 types of AVRT
-
Orthodromic: (most common) conduction goes down the AV node (often resulting in a narrow comlex unless aberrancy) and travels back to the atrium via the accessory pathway
-
Antidromic: conduction goes down the accessory pathway resulting in a broad, abnormal ventricular complex (often resembling VT) and back up to the atrium via the AV node.
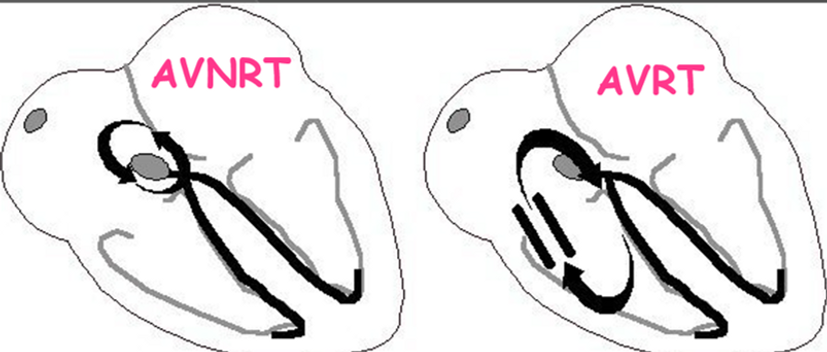
Atrioventricular node reentry tachycardia (AVNRT)

Atrioventricular reentry tachycardia (AVRT)



Junctional tachycardia
Tachycardia arising from the AV nodal junction.
Causes
-
Medication induced (Digitalis, Isuprel, etc)
-
Damaging AV junction (ablation, MI, rheumatic fever)
-
Electrolyte imbalance
-
Hypoxia

Wandering atrial pacemaker
Where multiple sites in the atrium (including the sinus node) are driving the rhythm.
Various p wave morphologies will be exhibited.
Rhythm is typically slightly irregular
Normal phenomena seen in high vagal tone (young, athletes or the elderly)





