CIED programming considerations during and after an AVN ablation
Pre ablation check
Perform normal check
Ensure all leads (most important V lead) are functioning well
•No sudden change in impedance, sensing, threshold
Ensure wound is healed well
•No hematoma, evidence of infection, etc
Reprogram to an appropriate mode for ablation
•Single chamber: VVI 30/40
•Dual chamber: VVI 30/40
AVN ablation procedure
1 sheath in femoral vein for ablation catheter +-2nd sheath if backup RV pacing catheter is used
Ablation catheter can be either non irrigated or irrigated, 4mm tip or 8mm tip (physician preference)
Ideally the AVN is ablated as opposed to the HIS - leaving a junctional escape rhythm
Diagrammatic view of the atrial septum in the right atrium to identify the various atrial nodal inputs to the atrioventricular (AV) node and His bundle. The fast pathway (yellow) runs along the anterior limbus of the oval fossa to enter the AV node (blue triangle), at the apex of which is the His bundle (red dot). The slow pathway runs from the coronary sinus (green area) to the AV node, whereas the central transitional cells traverse the area between the slow and fast pathways to input to the AV node.

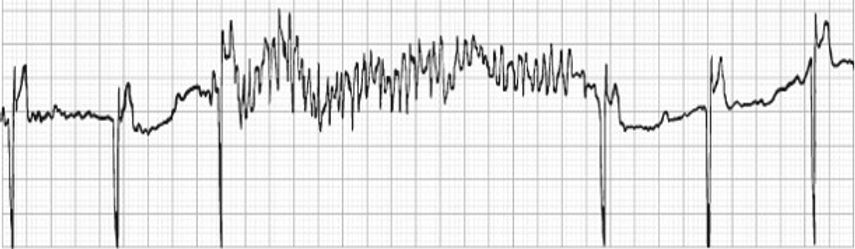
See rapid firing for the AV node during ablation follow by complete heart block

Potential risk of pacing inhibition during ablation
•Notify physician if this occurs
•Consider ASYNC if persistent
Post ablation check
Perform normal check
Ensure no changes in testing values
•Possible risk of lead damage during ablation
•Possible risk of moving lead with catheters
Ensure ablation has worked with VVI 40 / sensing testing
•In some circumstances when patient is in sinus rhythm, brief periods of AAI pacing may be required to prove CHB
Post ablation concerns
Increase in sympathetic activity post AVN ablation
Well documented risk of ventricular arrhythmias in the 1st few months following AVN ablation
•Particularly Torsades de Pointes
Post AVN ablation results in increased sympathetic nerve activity, increased cardiac action potential duration and increased effective refractory period.

Post ablation programming
Research has shown pacing at faster rates (e.g., 80 or 90 ppm) immediately post AVN ablation compared to standard rates (60 ppm), decreases sympathetic nerve activity
Ensure no algorithm is turned on which may violate the lower rate limit, as this may result in a long-short sequence
•The perfect recipe for Tosades
ICD therapies
•?SVT discriminators?
Poor programming example
Patient had a single chamber SJM PPM inserted prior to planned AVN ablation.
Was programmed to VVI 40 prior to ablation
V autocapture was turned ON to preserve battery and allow for trends of threshold
Had successful, uncomplicated AVN ablation
Device was reprogrammed to VVIR 80-120
Called ambulance due to persistent episodes of syncope and pre-syncope
Presenting rhythm
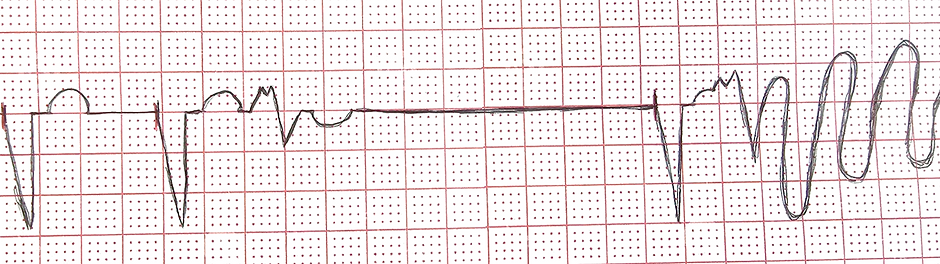
When V auto threshold is turned on in a SJM, if the device is a single chamber, or is a dual chamber with single chamber mode programming (VVI), a hysteresis automatically turns ON.
•Set 10ppm below current LRL.
•For this case mode was VVI 40, hysteresis goes to 30
The hysteresis rate was not turned OFF or changed during or at the end of the ablation
•VVIR 80-120
•Hysteresis 30
Algorithms that may violate LRL
Hysteresis
MVP modes
AV searches
Some autocapture tests (with no backup pulse)
NCAP
Rest rate/sleep rate
Post AVN ablation follow up
Book ~6 week post AVN ablation appointment with follow up clinic
Demonstrate whether the procedure was a success
•If recurrent, book for repeat ablation
Rates typically slowly titrated down (e.g., from 80 to 70)
Turn off all SVT discriminators
After 3 months consider restoring autocapture settings if they were turned off.
Post AVN ablation complications
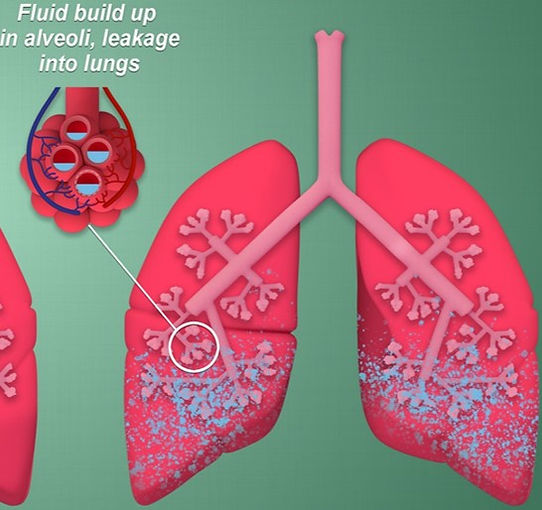
APO post AVN ablation – immediately or shortly after (up to 6 weeks post)
Studies have shown that this generally occurs due to worsening of MR
Usually due to the dilatation of the mitral valve annulus
•Due to slower rate
•Can be due to increased LV end
diastolic diameters (does not occur
in every pt)