Primary Prevention
Manage lifestyle factors to prevent AF occuring in those who are deemed high risk for developing AF.
obesity
physical inactivity
unhealthy alcohol consumption
smoking
diabetes
hypertension
Secondary Prevention
Management of comorbidities and risk factors for patients who have had AF.
obesity with BMI >27kh/m2 - aimed 10% weight loss
physical fitness - encouraged to do moderate-vigorous exercise for a target of 210 minutes/week
minimisation or cesssation of alcohol consumption
smoking cessation
caffiene abstention
screen for obstructive sleep apnoea
aiming for optimal BP control
Rhythm control
revert to SR/maintain SR
•Medications – Ia, Ic, III (Amiodarone, Sotolol, Flecainide)
•Cardiovert
•AF ablation – endocardial – RFA, cryo and PFA
•AF ablation - surgical

Rate control
accept AF – rate control (average V rate ~80 bpm)
•Medications – AVN blockers; Ca/Beta blockers (digoxin, Amio, Verapamil)
•Pacemaker and AVN ablation

Cardioversion
Performed under GA – requires anaesthetic team
Synced shock - ~150J
Factors effecting CV success
•Size of patient – obese patients may be difficult to revert
•Pad position – skin prep (hair may hinder)
•Duration of AF episode

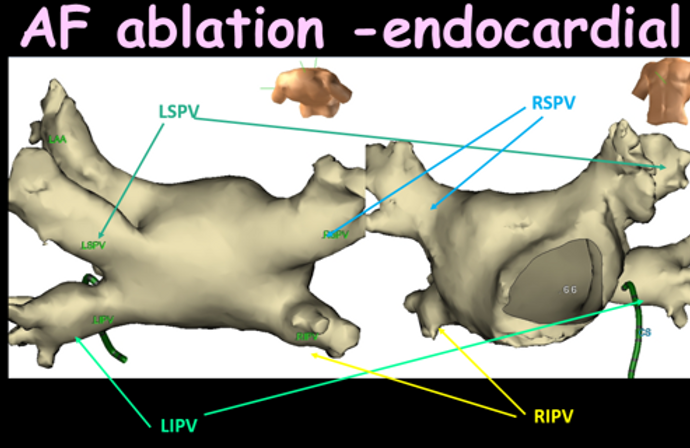
Endocardial ablation
Pulmonary vein isolation (PVI) is performed for paroxysmal AF using ablation technology. Back wall isolation may be used for persistent AF.
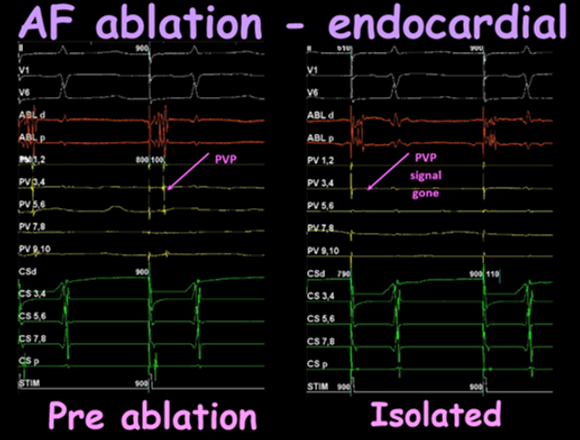
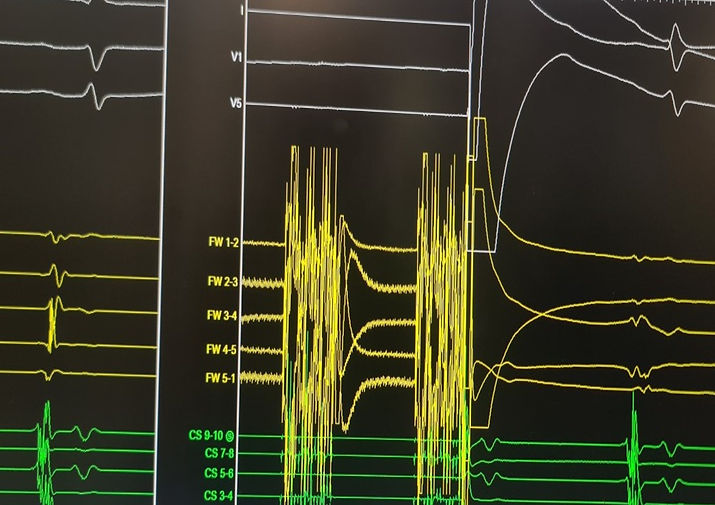
This image demonstrates pacing the atrium from the distal coronary sinus. Pre ablation the left atrium conducts into the pulmonary vein (pulmonary vein potential (PVP)). Once isolated, the PVP is gone demonstrating electrical isolation in the pulmonary vein.
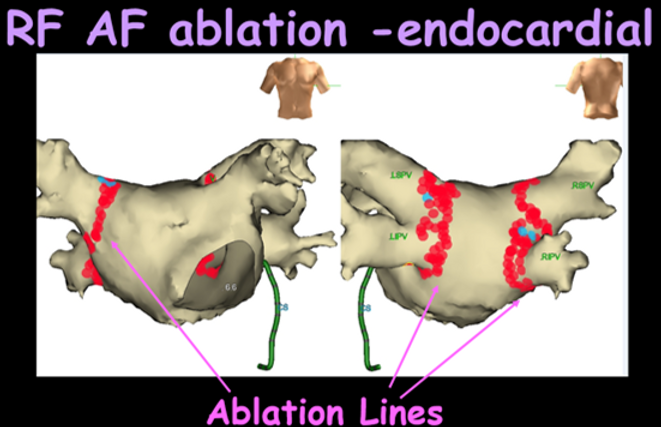
Radiofrequency (RF) ablation
Veins are isolated by application of hot temperatures using point to point ablation which causes permanent myocardial damage.
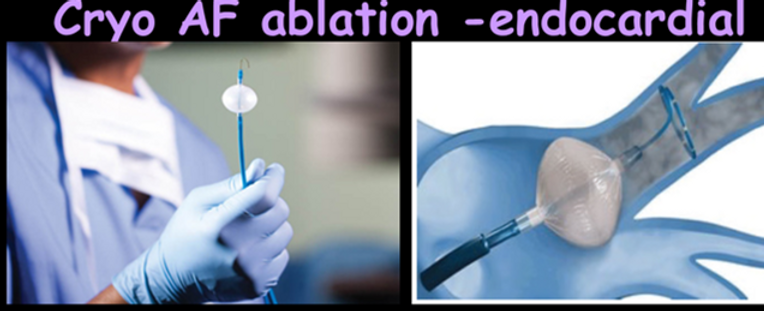
Cryothermy ablation
Veins are isolated by application of very cold temperatures via a balloon catheter which causes permanent myocardial damage.
Pulsed field ablation (PFA)
Veins are isolated by using PFA which is tissue specific (has no risk damaging surrounding tissues (e.g., oesphagus, phrenic nerve, etc)) by causing electroporation by increasing membrane permeability.
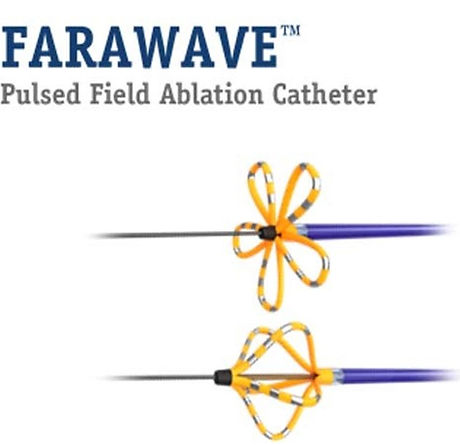
Boston Scientifics Farapulse PFA catheter. The flower pose (top) is used to ablate the antrium of the pulmonary veins, whilst the basket pose (bottom) is usd to ablate the ostirum of the pulmonary veins.
Surgical AF ablation
MAZE
•Cox MAZE
•TT MAZE (totally thoracoscopic)
Converge
Cryoablation after mitral valve surgery
Converge
•Pericardioscopic approach from upper abdomen
•Epicardial ablation of PVIs & LA posterior wall
•Block confirmed with endocardial system
•Beneficial for long standing persistent AF

MAZE
A series of ablation lesions are performed in the right and left atrium (including the pulmonary veins).

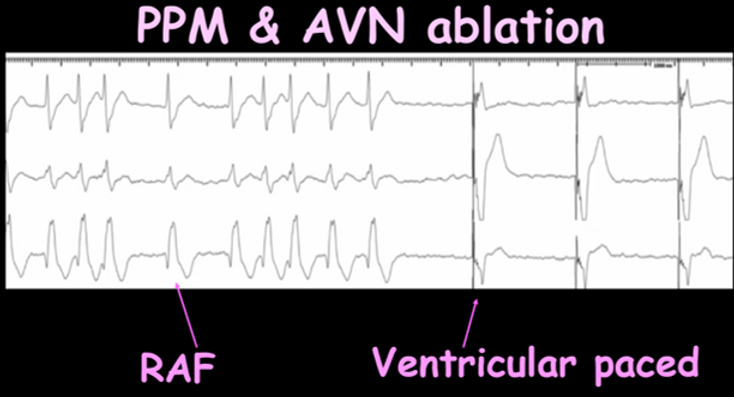
Permanent rate control
CIED is inserted prior to AV node ablation. After the ablation the ventricular rate is completely controlled by the pacemaker. Can be in sinus rhythm (PAF) or permanent AF.
Medications for AF
Reversion/maintenance of sinus rhythm
•Amiodarone
•Sotolol
•Flecainide
Rate control medications
•Amiodarone
•Digoxin
Anticoagulation
•Warfarin/Coumadin
•NOAC – Elliquis, Xarelto, Pradaxa
•LAA closure– left atrial appendage occlusion device
Stroke assessment risk
The CHADS-VASC risk score is often utilised when clinical AF is seen, to provide clarity whether a patient may need to be on anticoagulation.



Bleeding assessment risk
HAS-BLED score is a risk stratification score used to assess bleeding risk. Bleeding risk is usually assessed when anticoagulants are considered.

How much AF for anticoagulation?
Incidental/subclinical findings of AF on devices - ?significance of AF (subclinical AF (SCAF))
No randomised studies
Often up to doctors discretion – no consensus
Considered when stroke risk is high
Important Trials
•ASSERT trial (ASymptomatic Atrial Fibrillation and Stroke Evaluation in Pacemaker Patients and the atrial fibrillation Reduction Atrial Pacing Trial)
•NOAH-AFNET 6 Non-vitamin K antagonist Oral anticoagulants in patients with Atrial High rate episodes
ASSERT findings
•2012: duration (2 arms) of SCAF & stroke occurrence
•No SCAF or >6min SCAF
•Detection period was only 1st
3 months of implant
•>65 years
•Average CHADSVASC 2.3
•SCAF >6 minutes significantly higher
increase risk of stroke or embolic
event compared to no SCAF.
•However, duration of atrial high rate episodes in relation to stroke risk were not assessed

ASSERT findings - reassessed
•2017: duration (4 arms) of SCAF & stroke occurrence
•No SCAF
•>6 min SCAF
•>6 hours SCAF
•>24 hours SCAF
•2.5 year follow up period
•SCAF >24 hrs significantly higher increase risk of stroke or embolic event compared to SCAF <24 hours.
•There was no difference in embolic events/stroke in SCAF <24 hours & non AF groups

NOAH-AFNET 6 findings
•2023
•Mean patient age 78 years (all >65)
•37.4% female
•>6 minutes AF – median 2.8 hours
•Average CHADS-VASC of 4
•2 arms – placebo vs Edoxaban
•No reduction in CV death, stroke or systemic embolism
•Incidence of stroke was low in both groups
•Increase in major bleeding events
Alternative for anticoagulation
PROTECT AF
Percutaneous Left Atrial Appendage Closure vs Warfarin for Atrial Fibrillation
•Can be considered as an alternative for individuals who have high stroke risk but have contraindications to anticoagulants.





