ICDs
Ventricular arrhythmias
Ventricular tachycardia
>3 consecutive beats originating from the ventricle >100 bpm
•Sustained: >30 seconds or hemodynamic compromise <30 seconds
•Nonsustained: >3 beats, spontaneous termination

Torsades de Pointes
•PMVT generally associated with long QT, waxing & waning QRS amplitude. Usually follows long-short sequence

Ventricular Flutter
Regular, ~300bpm, sinusoidal, monomorphic appearance

Ventricular Fibrillation
Rapid (>300bpm), grossly irregular, marled variation in waveform

Subgroups of patients
Secondary prevention
Has had a previous ventricular arrhythmia/cardiac arrest.
ICD therapies superior to drug therapy alone in terms of mortality (SCD-HEFT, AVID, CASH, CIDs)
Primary prevention
Classified as high risk of having a ventricular arrhythmia
ICDs benefit the following groups in terms of mortality
•Inducible sustained VT in EP study (not VF) (MADIT)
•CAD or prior MI – ICM (MADIT II, MADIT)
•LVEF <30-40% (MADIT II, MADIT, SCD-HEFT)
•NICM (DEFINITE)
•Heart failure class II, III (SCD HEFT)
Ischemic Heart Disease (IHD)
Findings
AVID & CIDS
•2ndry prevention IHD pts
•Higher survival rate with ICD compared to med alone
•Mortality reduction 27%
SCD HeFT, MADIT II & MUSTT
•primary prevention
•Higher survival in ICD group
•Coronary artery spasm results from vasomotor dysfunction and can occur in the presence or absence of atherosclerotic IHD.
•Vasospasm episodes can lead to VA, syncope, and SCD.

Indications for secondary prevention IHD pts
Class I
•ICM, SCA due to VT/VF, hemodynamically unstable VT or sustained stable VT (no reversible cause) * (B)
•ICM, unexplained syncope, inducible sustained monomorphic VT on EP study* (B)
Class IIa
•SCA due to coronary artery spasm, medical therapy is ineffective/not tolerated* (B)
Class IIb
•SCA due to coronary artery spasm* (B)
Indications for primary prevention IHD pts
Class I
•LVEF <=35% IHD, 40days post MI/90days post revascularisation, NYHA II or III* (A)
•LVEF <=30% IHD, 40days post MI/90days post revascularisation, NYHA I* (A)
•NSVT due to prior MI, LVEF <=40%, inducible sustained VT/VF at EP study* (A)
Class IIa
•NYHA IV outpatients, transplant candidates/LVAD* (B)
Class III
•NYHA IV, medication refractory HF, not transplant candidates/LVAD or CRTD (C)
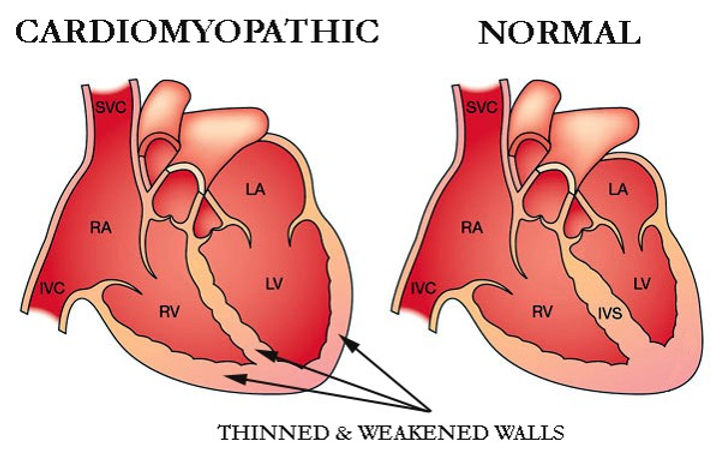
Non Ischemic Cardiomyopathy (NICM)
Many potential causes of NICM which are either
•Genetics
•Acquired
Leads to clinical manifestations of HF
•Fluid retention
•Dyspnoea
•Exercise intolerance
Indications for primary prevention NICM pts
Class I
•NICM, NYHA II-III, LVEF <=35% * (A)
Class IIa
•NICM due to Lamin A/C mutation with 2+ risk factors (NSVT, LVEF <=45%, nonmissense mutation, male) * (B)
Class IIb
•NICM, NYHA I, LVEF <=35%*(B)
Class III
•NYHA IV medication refractory HF, not transplant candidates/LVAD or CRTD (C)
Arrhythmogenic ventricular Cardiomyopathy (ARVC)
ARVC is an inherited cardiomyopathy that predominantly affects the RV but can affect the LV causing areas
of myocardial replacement with fibrosis and adipose tissue that frequently causes VA and SCD.
Indications
Class I
•ARVC with 1+ marker (SCA, sustained VT, significant ventricular dysfunction with RVEF or LVEF <35%)* (B)
Class IIa
•ARVC and syncope presumed to VA* (B)

Hypertrophic Cardiomyopathy (HCM)
Patients with HCM have approximately a 1% risk of SCD per year.
Some Risk Factors include
•VA with syncope
•FHx SCD w HCM
•NSVT >2beats
•LV wall thickness >29mm
•Unexplained syncope
•Abnormal BP response during exercise
Indications
Class I
•HCM, SCA due to VT/VF or have had spontaneous sustained VT causing hemodynamic compromise* (B)
Class IIa
•HCM with 1+ risk factor (max LV wall thickness >=30mm (B), SCD in 1+ 1st degree relatives presumed by HCM (C), 1+ episodes of unexplained syncope in last 6 months (C))*
•HCM spontaneous NSVT (B) or abnormal BP response with exercise (C) who have additional SCD risk modifiers or high risk features (C)*
Class IIb
•HCM with NSVT (B) or abnormal BP with exercise (B) but no other SCD risk modifiers (B)
Class III
•HCM genotype in absence of SCD risk factors (B)

Cardiac Sarcoidosis
Systemic granulomatous disease of unknown cause
Cardiac manifestations include conduction abnormalities, VA, and depressed ventricular function with or without HF
Indications
Class I
•Cardiac sarcoidosis with sustained VT or SCA with LVEF <=35% * (B)
Class IIa
•Cardiac sarcoidosis LVEF >35% with syncope and/or evidence of myocardial scar on MRI or PET with pacing indication* (B)
•Cardiac sarcoidosis LVEF >35% with inducible VA on EP study* (C)
•Cardiac sarcoidosis with pacing indication (C)

Neuromuscular Disorders
The muscular dystrophies are a group of inherited diseases affecting skeletal and cardiac muscle.
Some present primarily as a NICM while others present primarily as conduction system degeneration with a variable association with cardiomyopathy
Indications
Class I
•Neuromuscular disorders, primary and secondary prevention ICDs with same indications for pts with NICM * (B)
Class IIa
•Muscular dystrophies (Emery-Dreifuss or limb-girdle type IB) with progressive cardiac involvement * (B)
Class IIb
•Myotonic dystrophy type 1 with pacing indication * (B)

Long QT
There are 3 categories of long QT associated with different genes
•Type I KCNQ1
•Type II KCNH2
•Type III SCN5A
VA associated with long QT is often Torsades
T wave alternans is a major marked of cardiac electrical instability
And sinus pauses should be treated with concern
LQTS criteria
•>=480ms long
•460-479ms female prolonged for female
•450-459ms male prolonged for male
Other criteria used to diagnose include QTc >480ms 4 mins post exercise, torsades, T wave alternans, low heart rate for age, syncope, FHx, FHx unexplained SCD (<30yo)
Indications
Class I
•High risk symptomatic long QT, where beta blocker is ineffective/not tolerated (B)
Class IIb
•Asymptomatic long QT resting QTc >500ms while on beta blocker (B)

Short QT
QT =<340ms
Prevalance: 0.05%
More likely to have nocturnal episodes
Generally are medically managed (quinidine to prolong QT).
Indications
Class I
•Short QT with cardiac arrest or sustained VA * (B)

Catecholaminergic polymorphic VT (CPVT)
CPVT is characterised by exertion-related polymorphic/ bidirectional VT associated with syncope & SCA.
SCA/SCD is reported in 3% to 13% of pts
Indications
Class I
•CPVT with recurrent sustained VT or syncope, while on adequate maximally tolerated beta blocker (B)

Brugada/channelopathies
Brugada is a sodium channelopathy
Associated with gene mutations
Abnormal ECG appearance
•Incomplete RBBB
•ST elevation of saddle back appearance in anterior leads
Normal cardiac structure
Indications
Class I
•Cardiac channelopathy and SCA * (B)
•Brugada with spontaneous type I, cardiac arrest, sustained VA or recent hx of syncope (presumed to VA) * (B)

Early Repolarisation Syndrome
Significance is poorly understood.
•Initially thought to be significant
•Revised to benign
•Revised to significant
Occurs in up to 13% of the population
Abnormal ECG appearance
•J point/ST elevation in 2 or more contiguous leads
Indications
Class I
•ERP and cardiac arrest or sustained VA * (B)

Adult Congenital Heart Disease
Indications
Class I
•CHD and hemodynamically unstable VA after evaluation and appropriate tx for residual lesions/ventricular dysfunction * (B)
•CHD with SCA due to VT/VF wth no reversible causes * (B)
Class IIa
•Repaired tetralogy of fallot with inducible VT/VF or spontaneous sustained VT * (B)
•Repaired moderate or severe complexity CHD with unexplained syncope and at least moderate ventricular dysfunction or marked hypertrophy and inducible sustained VT in EP study (B)
Class IIb
•CHD severe ventricular dysfunction (LVEF <35%, symptoms of HF despite GDMT or additional risk factors * (B)

Idiopathic polymorphic VT/VF
Indications
Class I
•Resuscitated from SCA due to idiopathic PMVT or VF * (B)
Other
Details
Patients with HFrEF are at an increased risk for VA and SCD.
The risk is increased irrespective of HFrEF etiology
Development of disease in the transplanted heart places some patients at an increased risk of SCD that has ranged from 10% to 35% in observational studies Both rejection and a decreased LVEF are predictors of SCD.
The mechanisms underlying SCD in patients with a heart transplant include damage to the conduction system itself and VA due to coronary vasculopathy or during episodes of acute rejection.

LVAD: Left Ventricular Assistance Device
Used for pts with end stage HF
LVADs are surgically implant and are a battery-operated, mechanical pump, which helps the LV pump blood to the rest of the body.
Patients with an LVAD have a high risk of VA, particularly those with a history of arrhythmias.
increased risk may be due to myocardial irritation from insertion of the LVAD inflow cannula, LV compression due to a suctioning effect from the LVAD, inotropic support frequently needed by some patients, & repolarization changes that can occur after LVAD placement.

Indications
Class IIa
•LVAD and sustained VA (C)
•Older pts with significant comorbidities with primary prevention indications* (B)
•Heart failure reduced EF, awaiting hearts transplant who otherwise do not quality for ICD (e.g, NYHA IV) (B)
•Heart transplant and severe allograft vasculopathy with LV dysfunction* (B)
Class IIb
•Giant cell myocarditis with VF or hemodynamically unstable VT tested according to GDMT* (C)
Subcutaneous Defibrillators (ICD)
Indications
Class I
•ICD criteria, inadequate vascular access or high risk of infection, brady/CRT pacing or ATP for VT is neither needed nor anticipated (B)
Class IIa
•Meet ICD indications, brady/CRT pacing or ATP for VT is neither needed nor anticipated (B)
Class III
•Bradycardia/CRT indication or when ATP for VT is required (B)
transplant who otherwise do not quality for ICD (e.g, NYHA IV) (B)
•Heart transplant and severe allograft vasculopathy with LV dysfunction* (B)




