Complications of implant
Pocket related complications
Bruises/ecchymoses/hematoma
•More likely when on blood thinners
•Usually self resolve/dissipate
•May need a pocket wash out – infection risk

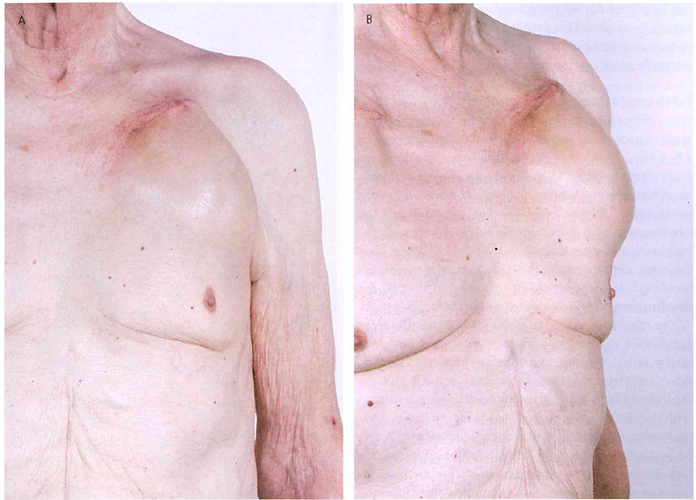
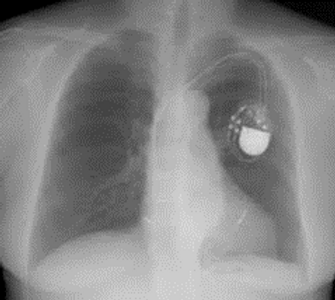
Device migration/erosion/infection
•Late complications include erosion and migration which often result from suboptimal initial surgery or infection.
•Errosion occurs in 5 different situations
•patient has an indolent infection
•pocket was too small at time of surgery
•IPG is implanted too superficially, especially in children or thin adults (lack of adipose tissue)
•IPG is implanted too far laterally in the anterior axillary fold
•The lead has been sutured to the subcutaneous or subcuticular tissue
•If an infection is suspected/occurs, the patient will have
•Antibiotics and
•Deeper infection – complete device removal/extraction

Chronic pain & painful pocket
•Initial local discomfort at the pacemaker implantation site is normal.
•This usually subsides and can usually be managed with mild analgesics (paracetamol)
•Others reasons pain may occur may be due to
•Infection
•Pacemaker implanted too superficial
•Pacemaker implanted too laterally
•Pacemaker allergy
•Infiltration of local anaesthetic in the deltopectoral groove (lateral incision) may result in injury to the thoracoabdominal nerves and result in chronic pain
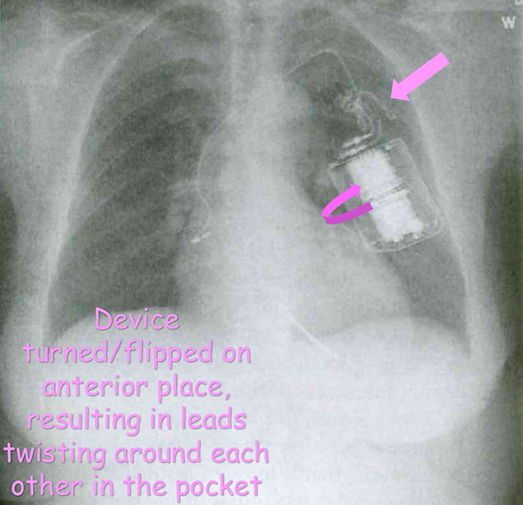
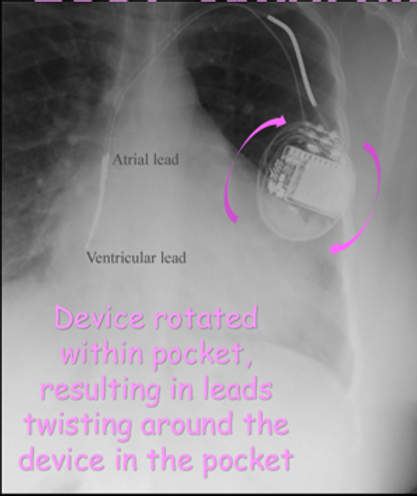
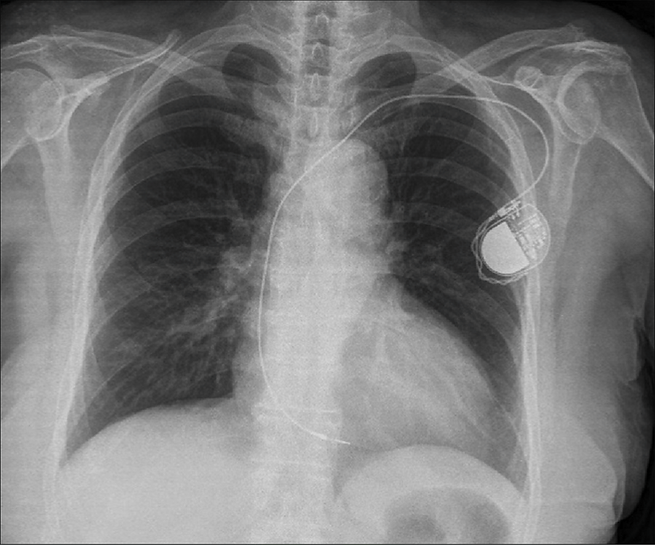
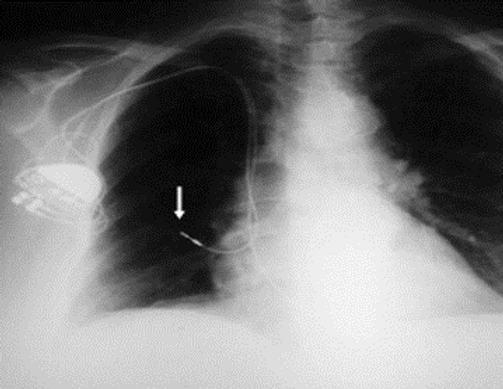
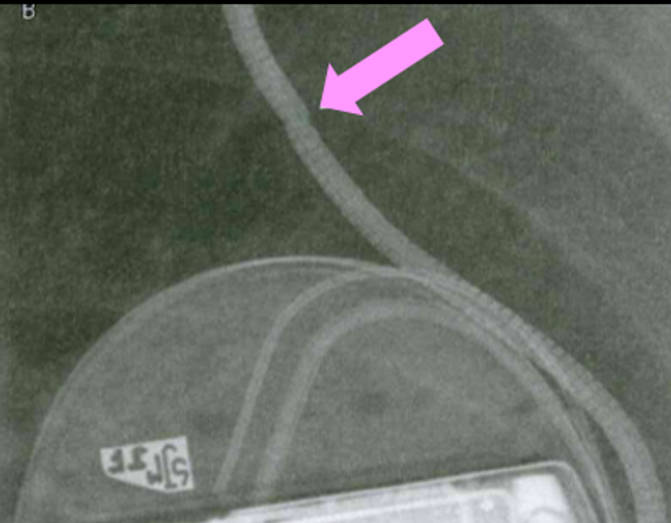
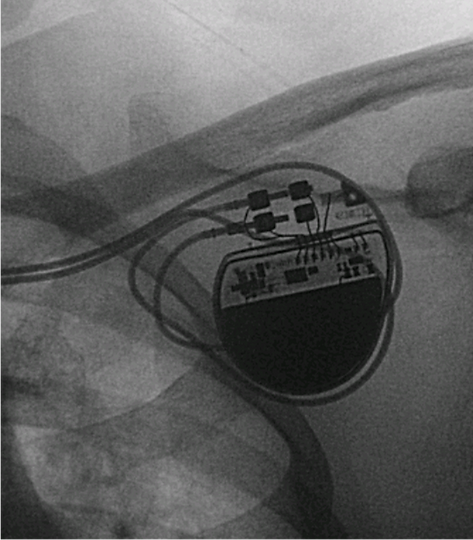
Twiddlers/reel syndrome
•Purposeful or absentminded manipulation of the pulse generator
•May result in
•Axial rotation of the device
•Twisting of the leads
•Potentially dislodging the leads
•More likely to occur with a loose pocket
•Predispositions include obesity & neuropsychiatric illnesses
•Usually requires lead re-implantation
•Device should be sutured down
Lead/access related issues
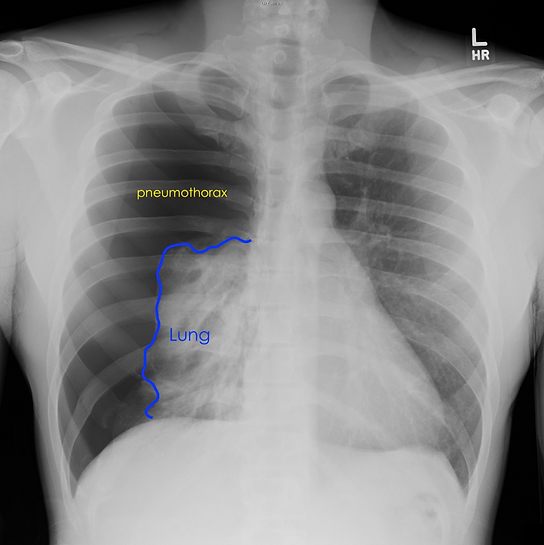
Pneumothorax
•Collapsed lung due to air between lung and chest wall
•May manifest during a case or up to 48 hours post implant
•Subclavian access poses a higher risk
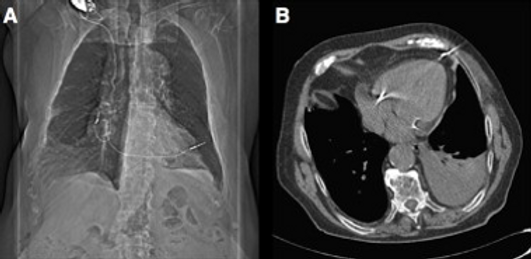
Lead dislodgement
•Most likely to happen within 1st few months of implant
•Micro dislodgments – not seen on x-ray
•Macro dislodgements – obvious on x-ray
•Likely requires a lead reposition/new lead
Lead perforation
•RA and RV free wall thin
•Elderly women highest risk of lead perforation
•May result in no significant change in testing values
•May result in lead reposition/ replacement
Damaged leads
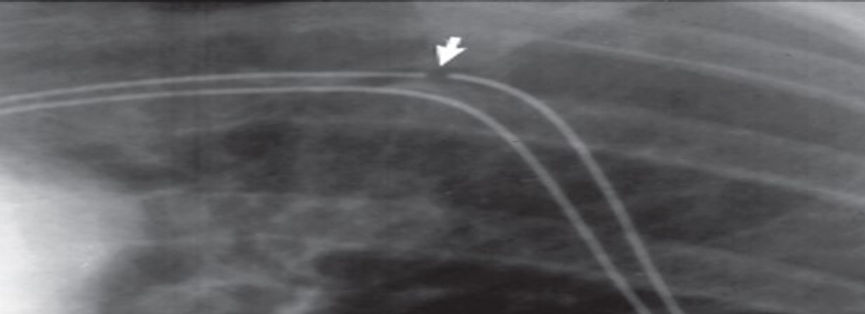
•Lead fractures
•Lead insulation breach
•Requires new lead
•May result in no output (if pt dependent)
•Inappropriate ICD shocks
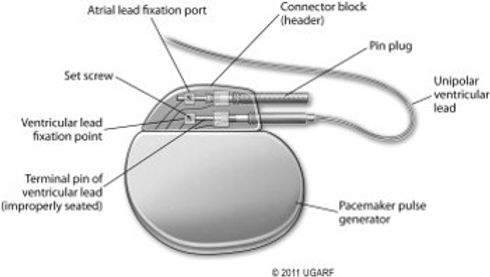
Inadequate lead connection at header
•Lead not screwed in properly
•Piston effect
•if there is any air in the device header prior to the lead being screwed in, there is a potential for the piston effect to put pressure on the lead which may move the lead slightly in the header
Pericarditis/tamponande
•May be associated with lead perforation.
•Pericarditis may occur without perforation.
•It is possible that an RA lead tip may irritate the pericardium.
•If there is no evidence of tamponade or symptomatic pericardial effusion, it is reasonable to treat pt conservatively (observation and pain medications) otherwise pericardiocentisis may be required
•Anti-inflammatory drugs or steroids, may relieve symptoms.
•If medications cannot be withdrawn without symptom reoccurrence, it may be necessary to remove and reposition the lead.
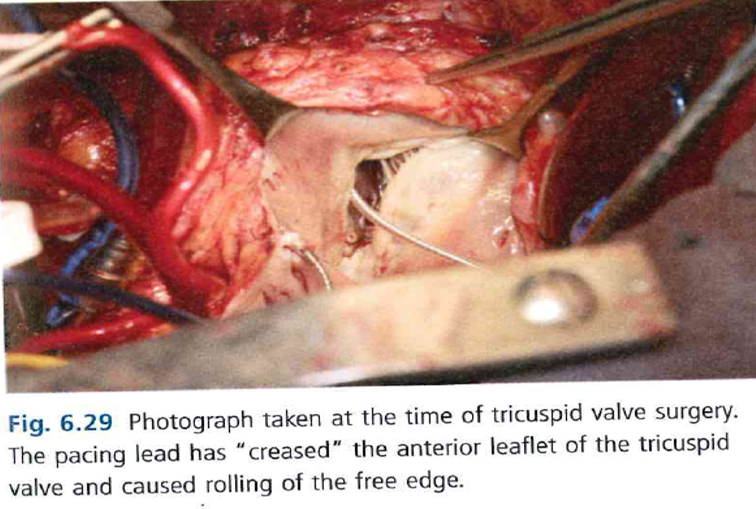
Tricuspid valve damage
•New onset TR can be due to RV lead implantation
•Studies have shown TR worse in 18-24% of pts
•Reasons for TR due to RV lead include
•Lead impingement of the valve
•Lead adherence to the valve
•Valve perforation by the lead and
•Lead entanglement
•Lead induced TR can be minimised by smaller lead diameter, alternative lead location (CS, RVOT)
•Very rarely, lead induced tricuspid stenosis has been reported secondary to subvalvular loop and subsequent adhesion.
Extra cardiac stimulation
•Diaphragmatic (direct diaphragm or phrenic nerve), pectoral muscle or intercostal muscle stimulation
•Most common in LV leads
•Usually can program around – vector change, output adjustment
•Tend to be positional
•Can also occur with
•high output unipolar lead settings
•Lead insulation issues
•Current leakage at device
•Not dangerous but very uncomfortable
Development of exit block
•Progressive threshold increase usually accompanied with progressive impedance rise
•Thought to be due to calcification development at lead tip

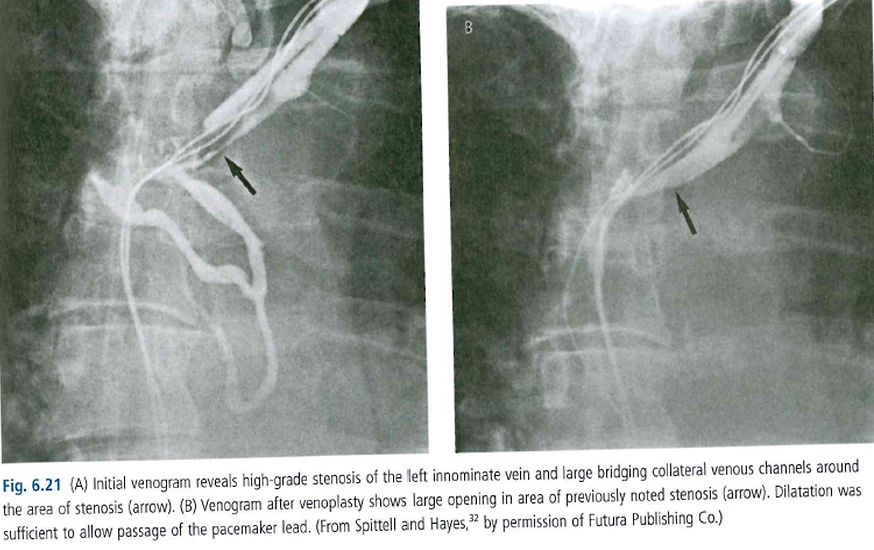
Thrombosis
•low risk 0.6-3.5%
•asymptomatic lead-associated thrombosis is more frequent
•some studies have shown with TOE 9% RA or SVC thrombosis, and 20% subclavian or innominate vein thrombi.
•Thrombus can lead to occlusion of the SVC, SVC syndrome, thrombosis of the SVC, RA or RV, with hemodynamic compromise or pulmonary embolism and symptomatic thrombosis of the subclavian vein with an edematous painful upper extremity.
•Partial or silent thrombosis is common and usually insignificant, except at time of pacing system revision, an alternative venous access may be required.
•Venoplasty may need to be used.
•Conservative treatment with bed rest, arm elevation and therapeutic anticoagulation often results in symptom relief.
Arrhythmias
•Arrhythmia's may occur during implant (all generally temporary)
•Atrial arrhythmias when positioning the atrial lead
•Ventricular arrhythmias when positioning the ventricular lead
•Heart block if pre-existing left bundle exists and right bundle is disturbed during RV lead implant
•Heart block if AV node is bumped during lead implantation
•Arrhythmias may occur post implant
•Sometimes ventricular leads, more likely LV leads, may cause ventricular arrhythmias (arrhythmogenic tissue) & may be required to turned off or repositioned
Device related complications
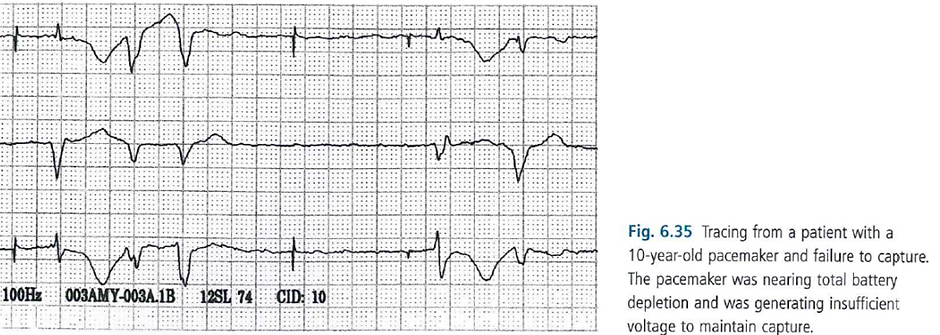
Battery depletion
•Normal/Abnormal
•Batteries don’t last forever (~10 years)
•Requires a generator change
•Premature battery depletion can be monitored by comparing battery estimate with previous checks estimate
ABNORMAL BEHAVIOUR
•At end of life, devices may display abnormal behaviour.
•The most serious and concerning behaviour known to have occur is known as “runaway pacemaker”
•This is when the device paces and a faster rate than programmed, sometimes even in rates the are non physiological.
•E.g., 300 bpm à risk of arrhythmia induction
•Device factory reset
•Possibly due to device fault
•Possibly due to external interference with device
•Results in suboptimal settings
•E.g., VVI 60 in a dual chamber pacemaker results in
•Possible unnecessary ventricular pacing
•Loss of AV synchrony
•No rate response
Poor programming/device related arrhythmia
Pacemaker arrhythmias
•PMTs
•RNRVAS
•AF
Unnecessary ventricular pacing
•AF
•LV dysfunction
•Heart failure hospitilisation
Inappropriate programming of algorithms that may cause pacing below the lower rate
•Pauses
•Torsades




