Sensing
ICDs must be able to accurately and reliably sense cardiac signals (to detect possible arrhythmias)
VF is characterized by low-amplitude signals
To reliably sense VF, the ICD would have to be so sensitive that it would likely also oversense P-waves, T-waves, and even pick up other signals in the body (myopotentials)
ICD sensing uses sophisticated adapting sensing algorithms

Sensing Example (Abbott)
For the purpose of explaining the complexities of sensing in and ICD, Abbotts "Sense ability" will be explained.
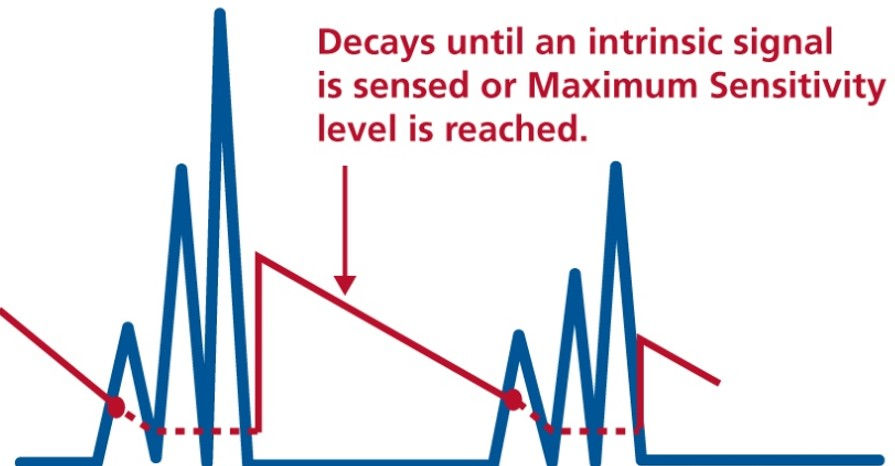
Sense ability is a dynamic sensitivity that changes as the patient’s intrinsic signals change
•Four key parameters
•Threshold Start
•Decay Delay
•Maximum Sensitivity
•Refractory Periods
Incoming Signals
The ICD gets its signal from the intracardiac electrogram
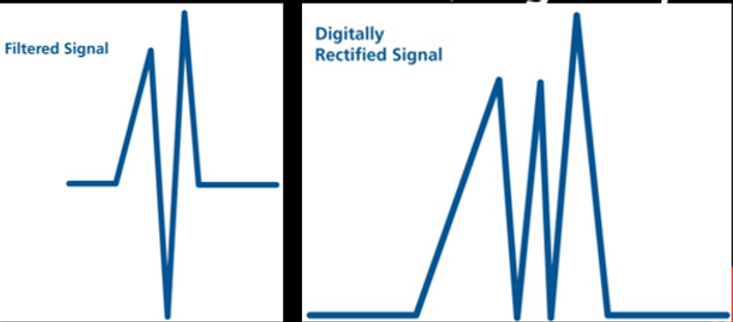
This EGM signal is filtered (to remove extraneous noise and far-field signals)
Then the filtered signal is digitally rectified so that all deflections are positive from the baseline
SenseAbility works with this filtered, digitally rectified signal
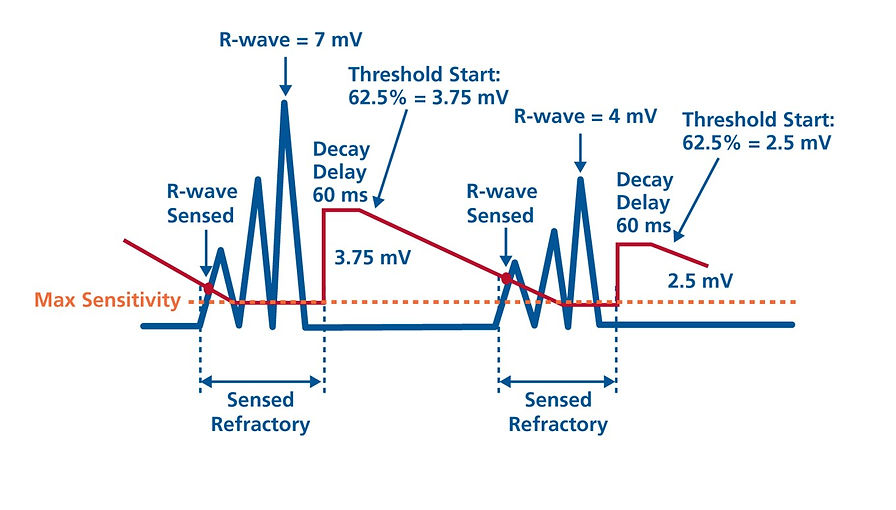
Determining the peak amplitude
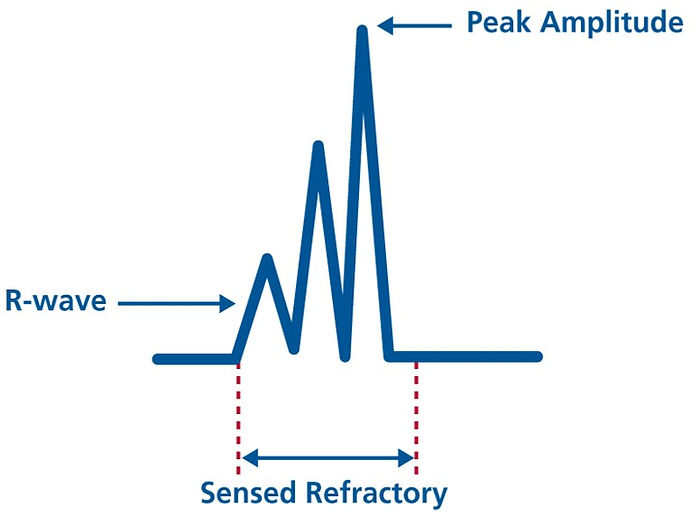
The sensed refractory period is programmable
•93, 125 or 157 ms in atrium
•125 or 157 ms in ventricle
Peak amplitude is the maximum amplitude that occurs during the sensed refractory period
The value of the peak amplitude is stored and used for the next Threshold Start
•Threshold Start is a percentage
of the peak amplitude
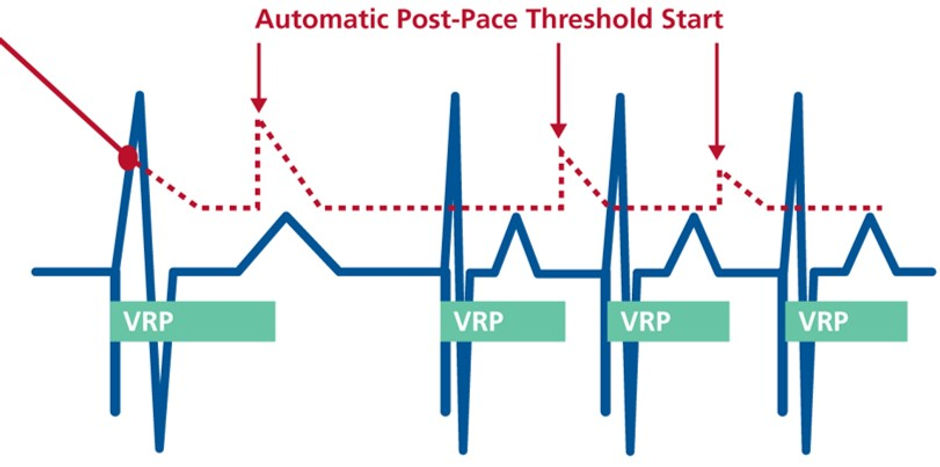
Threshold start
Adjusts the sensitivity setting based on intrinsic signals
Device resets sensitivity each cardiac cycle
Every new sensitivity setting begins with threshold start
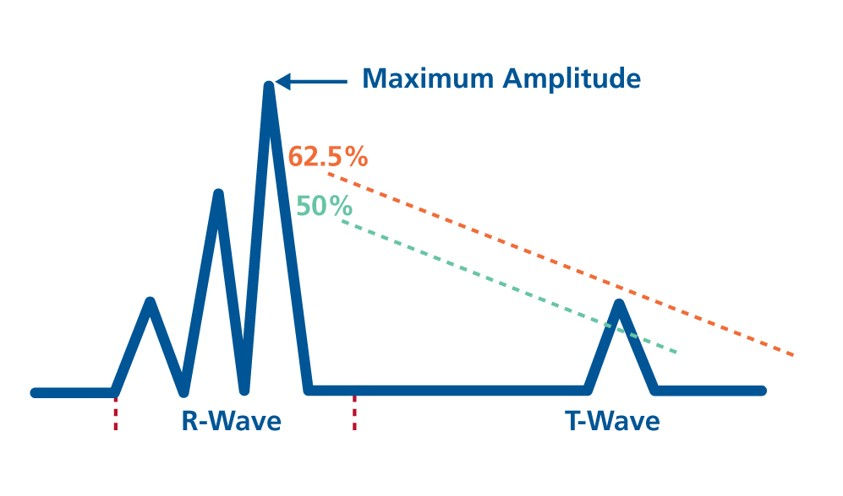
Threshold start is a programmable percentage of the peak amplitude (nominal 62.5%)
Threshold start is used to being the linear decay
As paced rate increases, Threshold Start automatically decreases (becomes a smaller and smaller percentage)
This allows the ICD to become increasingly sensitive at higher rates
Linear decay
If Threshold Start was programmed to 50%, it would sense the T-wave in this example
However, if Threshold Start was programmed to 62.5% (nominal) it would not “see” the T-wave
Careful programming of Threshold Start can help prevent T-wave oversensing
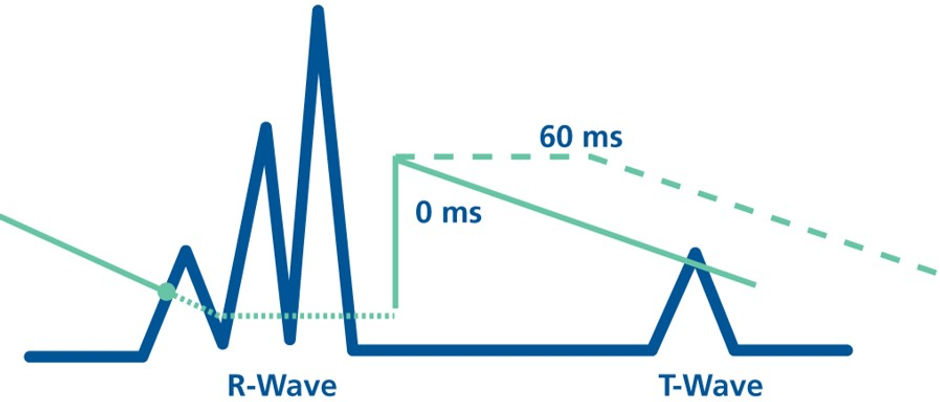
Decay Delay
Decay Delay is programmable in ms
It delays the time before the linear decay occurs
In this example, a 60 ms Decay Delay allows the ICD to miss the T-wave
Had no Decay Delay been programmed, the ICD would have oversensed the T-wave
Post-sensed Decay Delay values are fixed values
Post-paced Decay Delay values can be fixed or AUTO (for ventricle)
When AUTO is used, the device bases Threshold Start and Decay Delay on the pacing rate (since there is no intrinsic signal to measure)
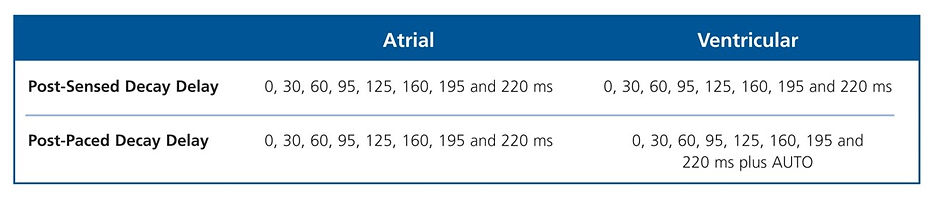
Maximum Sensitivity
Defines most sensitive level the ICD can reach
Signals that fall below Max Sensitivity cannot ever be sensed
Programmable/nominal values
•0.2 mV for atrium
•0.3 mV for ventricle
This parameter governs the ICD sensing only
•Separate maximum sensitivity
setting for brady
SenseAbility in action
Benefits of SenseAbility
SenseAbility™ technology gives control over ICD sensing without making ICD sensing unnecessarily complex
•Only four key parameters
•Allows flexibility to help troubleshoot oversensing
SenseAbility changes sensitivity on every beat so it adjusts as your patient’s intrinsic activity changes
Available in atrium and ventricle
•Atrium offers option of fixed sensitivity or SenseAbility
•Ventricle offers option of programmed or AUTO post-paced Decay Delay
Programming Considerations
Nominal settings are considered appropriate for the majority of patients
SenseAbility™ settings can be adjusted to help troubleshoot
•T-wave oversensing
•Far-field sensing
•Myopotential sensing
Consider AUTO post-paced Decay Delay for patients who are frequently paced at sensor-driven rates
Troubleshooting
Oversensing
•Program a higher Threshold Start percentage
•Program the Decay Delay (or extend it)
Undersensing
•Program a lower Threshold Start percentage
•Reduce the Decay Delay (even to 0, if need be)
Sensing problems at high paced rates (while patient is active) but not otherwise
•Program AUTO post-paced Decay Delay
Medtronic T wave discrimination example
Differentiates R-waves from T-waves by analysing differences in amplitude, frequency content, and patterns
Reduces the chance of inappropriate shocks due to TWOs but doesn’t stop TWOs occurring
R waves are generally higher frequency (faster) compared to T wave signals (slower)
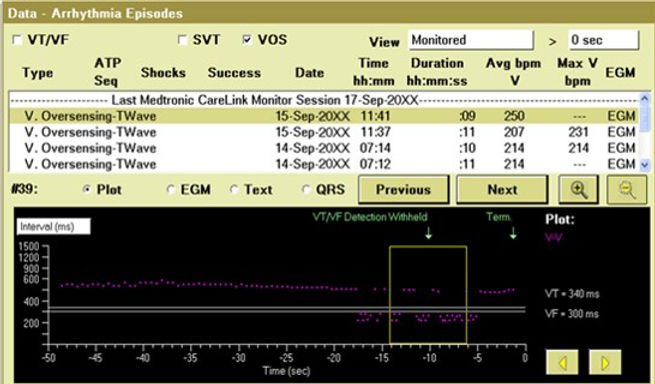

Medtronic T wave discrimination example





