Defining Heart failure
What is heart failure
A syndrome that results in a constellation of symptoms that can result from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood.
•SOB
•Fatigue
•Edema
•fluid accumulation
Types of heart failure
Acute HF: new onset HF or worsening HF resulting in dangerous symptoms such a pulmonary r peripheral congestion (or both).
Chronic HF: may have acute HF resulting in hospitalization
Decompensated HF: “failure to compensate.” Advanced form of HF due to overcompensation in early HF
Systolic HF: inability to eject blood effectively during the cardiac cycle (systole)
Diastolic: inability to fill effectively with blood prior to pumping (diastole)
Right sided/left sided HF: left sided more common
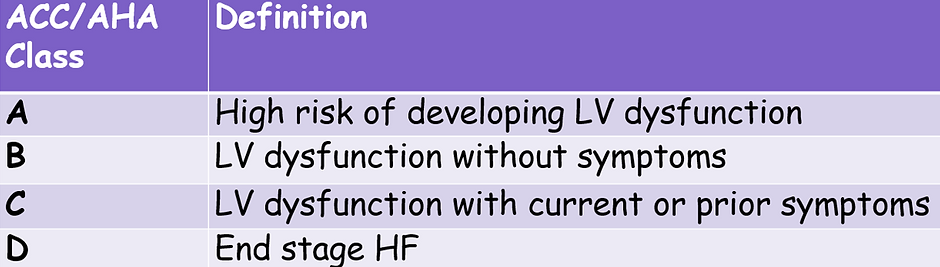
Classifying heart failure
LVEF can be used to classify HF severity
•HF with reduced EF (HPrEF): LVEF <40%
•HF with mildly reduced EF: LVEF 41-49%
•HF with preserved EF (HPpEF):LVEF >49%
•HF with improved EF:LVEF >40% which has previously been <40%

Causes of HF
Determining etiology of HF is important to help guide management strategies.
Coronary artery disease (CAD)/myocardial infarction: a build-up of fatty deposits and plaque in the coronary arteries/infraction resulting in scar
•2/3rds of HF pts have CAD
•All newly dx HF pts should have a coronary angiogram or CTCA
Valvular heart disease
•rheumatic heart disease (RHD) most common cause worldwide
•Australia RHD burden is 56 per 100 000
Cardiomyopathy: Dilated CM: large floppy muscle (usually idiopathic); HOCM: stiff thickened heart; sarcoid, cardiac amyloidosis, cardiac hemochromatosis, Takotsubo, Peripartum
Systolic and diastolic dysfunction: systolic dysfunction results in low EF <40. (LVEF = SV/LVEDV)
Non-ischemic heart disease:
•High blood pressure
•Metabolic diseases: diabetes and hypothyroidism
•Rhythm disorders: AF in particular
•Toxins (alcohol) or viral infection – rare
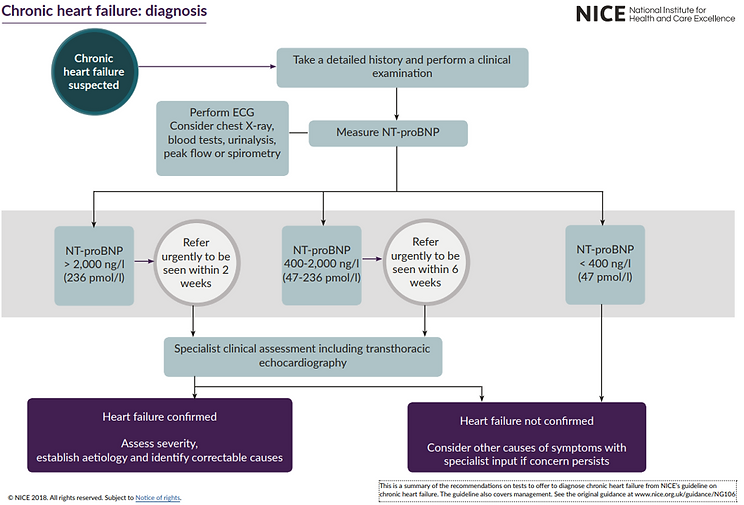
Diagnosing & managing HF
When chronic HF is suspected examinations and tests are performed to confirm diagnosis - see table below
Once HF is confirmed, severity is assessed, etiology is explored and correctable causes are identified.
According to severity of HF, a management plan is established - see treating heart failure
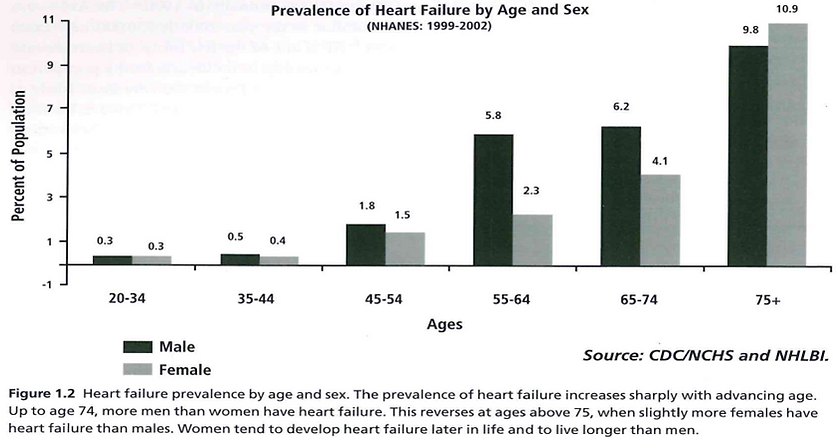
Incidence, prevalence & population of HF
Predicted to be 1-2% of Australians in recent years
This number is predicted to be much higher in Aboriginal and Torres Strait Islander communities
More common in older populations
•2/3rd of Australians with HF are >65 years old
Income factors
•Higher-income countries have higher rates of ischemic heart disease and COPD
•lower-income countries have higher rates of hypertensive heart disease, cardiomyopathy, rheumatic heart disease, and myocarditis.
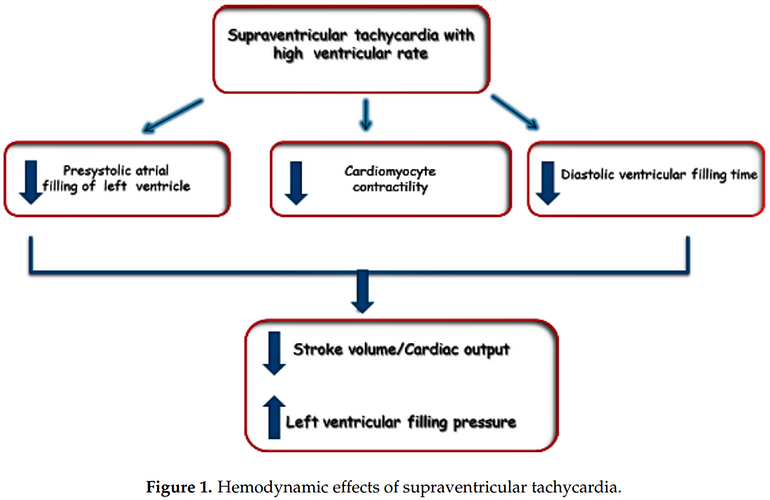
Arrhythmias in HF
Predisposition of HF patients developing arrhythmias
•Atrial arrhythmias – worsening HF symptoms (rapid V conduction)
•Atrial fibrillation
•Atrial flutter
•Ventricular arrhythmias – SCD risk
•VT/VF
•Bradyarrhythmias – worsening HF symptoms (dysnchrony) or resulting in syncope
•Sinus node dysfunction
•Tachy-brady syndrome
•Conduction disorders (AV nodal and BBB related)
•Sudden death (likely VA related) accounts for a significant proportion of total mortality in HF patients with II–III NYHA class
•Progressive hemodynamic deterioration and pump failure are the major causes of death in patients with IV NYHA class